Are BMI Surgery Qualifications Outdated?
The standard qualifications for being a candidate for bariatric surgery according to the National Institute of Health are as follows:
- BMI 40+ or 100 pounds higher-weight person, or
- BMI in the range of 35-40 and at least one weight-related condition, such as high blood pressure, non-alcoholic fatty liver disease, sleep apnea, type 2 diabetes, heart disease, etc.
The National Institute of Health established these qualifications in 1991. Did you know that someone built the first website in 1991 and put it online in August of that year? The first web browser did not become available to the public until 1993. Imagine if computer technology were still stuck in 1991! With all the advancements in technology, science, and medicine, the National Institute of Health is still using these standards.
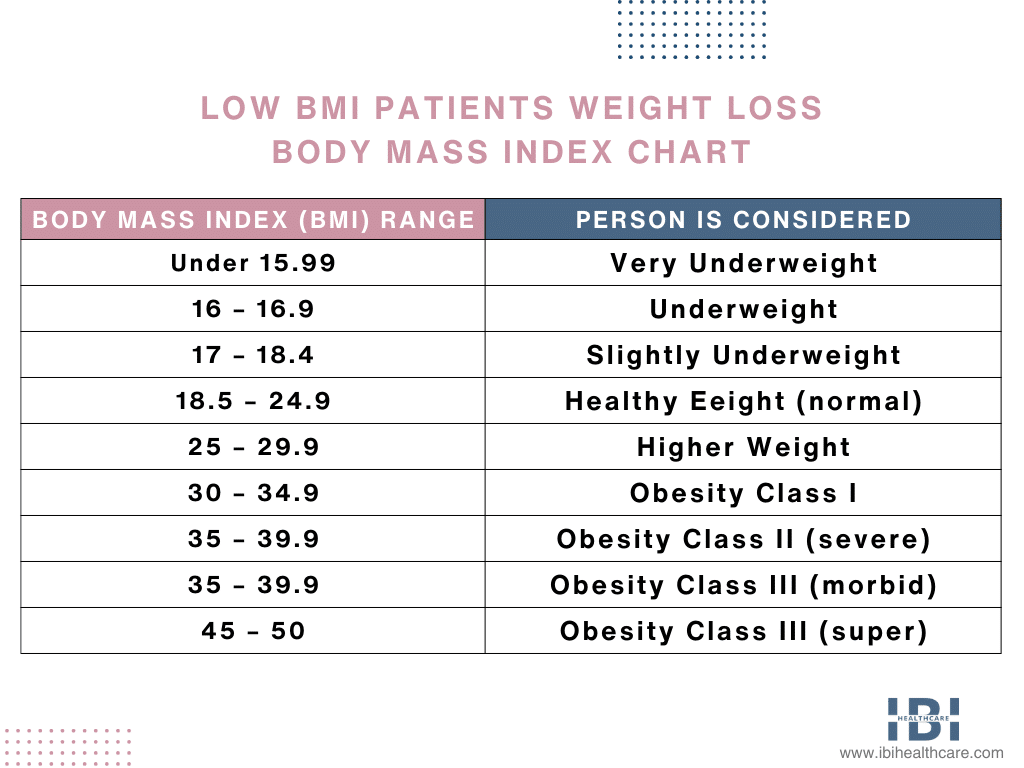
Here is an example of a BMI chart that outlines body mass index (BMI) ranges and associated categories.
BMI Patients Weight Loss Chart
Low BMI Patients Weight Loss – Metabolic Set Point
Today doctors know many things about our bodies but when it comes to weight loss, they are still trying to figure out why some individuals seem to have a much harder time losing weight and maintaining that weight loss than others. Studies have determined that our bodies have some sort of metabolic ‘set point’ when it comes to our weight.
While there is uncertainty about how this point is triggered, it is thought that large weight gains could influence it. Additionally, our “Western” diet or a combination of these consists of large amounts of processed foods, red meat, foods with high sugar content, high-fat dairy products, and pre-packaged foods.
When an individual starts dieting and exercising to lose weight. The body’s natural protection mode kicks in to preserve weight reserves by increasing the appetite and slowing down the metabolism, so it doesn’t burn fat as fast.
This just causes a yo-yo effect with gaining and losing weight and starts a vicious cycle. The individual can be left feeling defeated and weak because of their lack of willpower; but it is not their willpower at all, it is their own body working against them.
Bariatric surgery can be a very effective tool for weight loss and resetting the body’s “set point”. During weight loss surgery, the body’s processing of food changes, and it eliminates most of the sources of hunger-producing hormones. These changes can make our bodies stop working against us when we endeavor to lose weight.
Low BMI Patients and Bariatric Surgery
Several people are considered higher-weight people but fall outside of the bariatric surgery qualifications. These patients fall in the BMI range of 30-39.9 and can suffer from obesity-related health issues like type 2 diabetes, high blood pressure, sleep apnea, etc.
Yet, this group of Class I individuals would have to gain more weight to be allowed to use this proven tool of bariatric surgery to help them lose weight. It is baffling and I will give you a few reasons why.
The more weight an individual gains, the harder it is for them to lose it and maintain a healthy weight in the long run. Also, higher-weight individuals have more health problems, and one that occurs very frequently is type 2 diabetes.
Numerous studies have shown that bariatric weight loss surgery puts type 2 diabetes into remission in about 90% of cases. This means all these patients no longer need insulin or medicine to control their blood sugar. That adds up to a very big chunk of money saved by insurance companies and individuals for medication. It makes more sense to cure the disease by addressing the real problem than it does to treat a lifetime of symptoms.
Low BMI Patients Weight Loss – Endorsing Bariatric Surgery
The American Society Of Metabolic and Bariatric Surgery updated its position on qualifiers for weight loss surgery to include Class I patients. Since their publication, several other bariatric-specific organizations followed their steps (the International Federation for the Surgery of Obesity and Metabolic Disorders and The National Institute for Health and Care Excellence, UK).
At The Diabetes Surgery Summit (an international conference, where the leading diabetes organizations collaborated to pen global guidelines regarding bariatric and metabolic surgery to treat type 2 diabetes. The American Diabetes Association, The International Diabetes Federation, and 45 worldwide scientific medical societies formally endorsed the guidelines. The guidelines indicate that:
Individuals that fall into the Class I obesity category and experience inadequately controlled type 2 diabetes should be considered eligible for bariatric surgery.
Despite all the evidence indicating the benefits of including these lower BMI patients in the guidelines. The National Health Institute has yet to update its 1991 statement, which insurance companies use as their baseline.
Many advancements, new surgical procedures, and technological improvements in the field of bariatric surgery have occurred since these guidelines were published. These advancements, such as replacing open surgery with laparoscopic surgery, have significantly lowered the risks of bariatric procedures.
Low BMI Patients Weight Loss – Best Bariatric Surgery Options
The type of surgery that will work best will vary by patient and their unique circumstances. The American Society For Metabolic and Bariatric Surgery suggests Gastric Bypass and Sleeve Gastrectomy as good choices for patients with a BMI between 30 and 35.
One study conducted over 5 years made a good case for sleeve gastrectomy surgery in lower BMI patients reporting excellent results. In another study, researchers monitored patients with type 2 diabetes, hypertension, and sleep apnea after they underwent bariatric surgery.
Some patients with type 2 diabetes had laparoscopic gastric bypass and other patients had laparoscopic sleeve gastrectomy.
- 86% of the patients with type 2 diabetes experienced remission.
- 87% of patients with hypertension experienced remission.
- 100% of sleep apnea patients experienced remission.
The study concludes: “The results of our study support the validity of bariatric surgery in patients with BMI 30-35”.
Low BMI Patients – Non-Invasive Bariatric Procedures
Research has shown that early intervention directly relates to the longevity of the results. When it comes to weight loss surgery, especially in patients with type 2 diabetes. The patients had been experiencing type 2 diabetes for at least 5 years before bariatric surgery. They were more likely to not find relief after surgery or temporarily go into remission but flare up again in a few years.
This indicates that patients would benefit from weight loss procedures before health-related issues take root. Both gastric balloons and endoscopic sleeve gastroplasty may also be good options for patients in the BMI range of 30-34.9.
Gastric Balloons
There are a few different types of gastric balloons. Some are singular and in some cases, they use more than one balloon. Each system works by taking up space in the stomach, so the patient feels full from a smaller amount of food.
This helps patients reduce portion sizes and eat less. The medical team removes the balloon from the stomach after 6 months, and it is temporary. While the balloon is in the stomach, and for 6 months after its removal, the medical team provides patients with ongoing nutritional and behavioral sessions for support. At the IBI Healthcare Institute, we offer the Orbera® Gastric Balloon.
Endoscopic Sleeve Gastroplasty (ESG)
Endoscopic Sleeve Gastroplasty is a non-surgical procedure that reduces the stomach size through the use of sutures. Using an endoscope, the medical team accesses the stomach and blocks off about 75% of it, making it substantially smaller.
The smaller stomach helps patients to not overeat at mealtime and food takes a bit longer to digest. This helps them feel full for longer periods. The procedure only takes about 45 minutes, it does not require any incisions, there is no hospital stay involved, and the recovery is much shorter than surgery.
However, at the IBI Healthcare Institute, we individually evaluate patients and commit to helping everyone we can. Above all, if you or a loved one has a BMI in the range of 30-34.9. Nonetheless interested in bariatric surgery or a non-surgical weight loss procedure to regain health, please contact us today. Regardless, our team of experts can help you learn about procedures that will work for you. Lastly, give you all the information necessary to make an informed decision.









