What is a Paraesophageal Hernia?
In particular, a paraesophageal hernia occurs. When the lower part of the esophagus, the stomach, or other organs move up into the chest. The hiatus is an opening in the diaphragm. A muscle separates the chest from the abdomen through which organs pass from the chest into the abdomen.
The lower part of the esophagus and the stomach normally reside in the abdomen, just under the diaphragm. The gastroesophageal (GE) junction is the area where the esophagus connects with the stomach. Usually located 1 to 2 inches below the diaphragm.
A hiatal or paraesophageal hernia occurs. When the GE junction, the stomach, or other abdominal organs. Such as the small intestine, colon, or spleen move up into the chest where they do not belong.
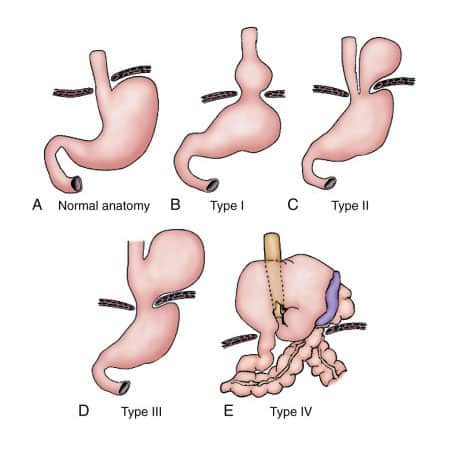
Even supposing, there are several types of paraesophageal hernias. Firstly, Type I is a hiatal hernia or sliding hernia. GE junction moves above the diaphragm, leaving the stomach in the abdomen. Thus, it represents 95% of all paraesophageal hernias. Secondly, Types II, III, and IV occur. When part or all of the stomach and sometimes other organs move up into the chest.
Paraesophageal Hernia - Common Symptoms
Indeed, more than half of the population has a hiatal or paraesophageal hernia. However, most people are symptom-free. Besides this, they may cause symptoms. For instance:

- Nausea.
- Bloating.
- Reflux and heartburn.
- Burping, and vomiting.
- Regurgitation of food.
- Food feels stuck in the chest.
- Sense of fullness after eating.
- Shortness of breath or coughing.
- Unexplained upper abdominal or chest pain.
However, severe symptoms occur for paraesophageal hernia. Particurlalry, when the bowel or stomach twists or loses its blood supply. These symptoms require immediate medical attention. Such as:
- Chest pain.
- Palpitations.
- Racing Heart.
- Severe vomiting.
- Shortness of breath.
- Severe abdominal pain.
- Lack of bowel movements.

Paraesophageal Hernia - Diagnosis
CT Scan
Doctors may incidentally identify a paraesophageal hernia during imaging. For instance chest X-ray, computed tomography (CT), or magnetic resonance imaging. In addition, patients with symptoms may undergo barium swallow. In this procedure, the patient swallows a contrast agent. Then a series of X-rays reveal the anatomy of the esophagus and stomach.
Upper Endoscopy
On one hand, doctors perform an upper endoscopy (esophagogastroduodenoscopy) as a procedure done under sedation. Generally, the doctor visualizes the anatomy of the esophagus and stomach to determine paraesophageal hernia. By inserting a thin camera to look at the upper gastrointestinal tract.
Manometry
On the other hand, doctors may use manometry to measure the severity of paraesophageal hernia. As well as associated diseases and established treatments. It allows measuring the pressure inside the esophagus. To determine if the muscles are too loose or too tight. Doctors may use a CT scan for surgical planning.
Paraesophageal Hernias - Available Treatments
Certainly, the treatment of paraesophageal hernias depends on the type of hernia and the severity of symptoms. Although, doctors typically manage type I hiatal hernias with medications for reflux. Hence do not require other treatment.
Whereas, Type II and III hernias may require surgery. Particularly, if they become symptomatic. However, in type IV hernias, organs such as the small bowel, colon, or pancreas can trapped in the chest. Eventually, the surgery is often necessary. Furthermore, depending on the type and severity of the hernia.
The surgical approach may be from the abdomen or the chest. Moreover, the operation is often minimally invasive with small incisions. But it may require open surgery.
Paraesophageal Hernia - Recovery Time
Because paraesophageal hernia is a major surgery, a full recovery can take 10 to 12 weeks. Nonetheless, patients can resume normal activities in less than 10 to 12 weeks. For example, you can start driving again as soon as you’re off narcotic pain medication.
As long as your job isn’t physically strenuous, you can resume work in about 6 to 8 weeks. Though, for more physically demanding jobs that require a lot of hard labor. It may be closer to three months before you can return. Call us or schedule a teleconsultation to inquire more about the Paraesophageal hernia repair surgery.






