Eosinophilic Esophagitis (EoE) is an inflammation of the esophagus. It’s been recognized as a major cause of GI symptoms in both kids and adults over the past 20 years. Knowing the causes, symptoms and treatment options is key to managing this condition or eosinophilic gastritis.
This guide covers the basics of EoE for those affected by it and those who want to learn more.
Eosinophilic Esophagitis (EoE) Overview
What is EoE and its Connection with White Blood Cells?
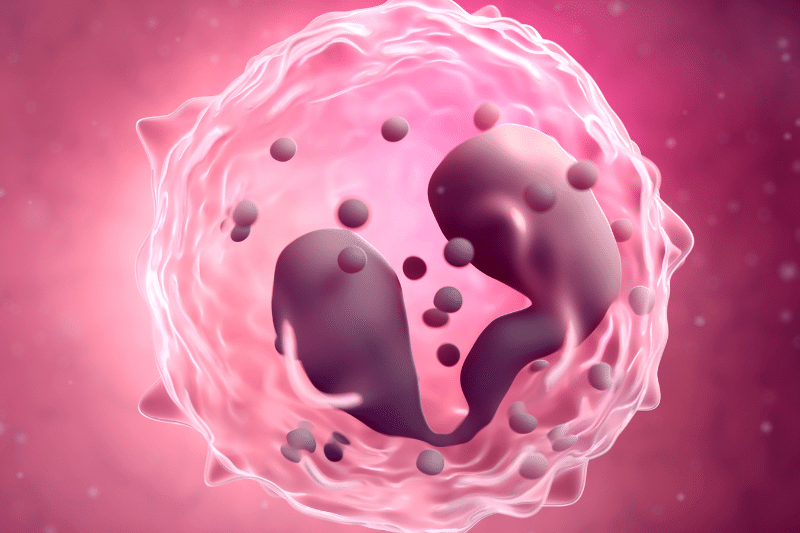
To better understand EoE, it is important to know that Eosinophilic Esophagitis (EoE) is a chronic immune system disorder. This condition is characterized by the accumulation of eosinophils. Particularly, a type of white blood cell, in the lining of the esophagus.
This accumulation causes inflammation and damage to the esophageal tissue making it hard for food to pass through. EoE was first recognized as a distinct condition in the early 90s and has been studied extensively since then.
EoE is often triggered by an allergic reaction or reactions to certain foods or environmental allergens. In addition, the exact cause of EoE is different from other esophageal conditions like gastroesophageal reflux disease (GERD) although they can have similar symptoms. Organizations and research initiatives aimed at enhancing the understanding and treatment of eosinophilic disorders, including EoE, play a crucial role in providing support, resources, and clinical research opportunities for affected individuals and their families.
What do Eosinophils in the Esophagus Mean?
Eosinophils are a type of white blood cell that helps the body fight infections and respond to allergies. When there are a lot of eosinophils or white blood cells in the esophagus it means the body is having an abnormal response, usually to an allergy. Eosinophils in the esophagus are the white blood cells called the hallmark of EoE, it’s what differentiates it from GERD where eosinophils are either absent or very few.
How Common is Eosinophilic Esophagitis?
EoE is considered a rare condition but its incidence is rising. According to recent stats, EoE affects 1 in 2,000 people in the US.
A 2023 study in The American Journal of Gastroenterology found that the incidence of EoE in the US is 57 per 100,000 people, men more than women. Worldwide it’s also becoming more commonly diagnosed especially in Western countries.
Is Eosinophilic Esophagitis Hereditary?
There is some evidence that EoE has a genetic component. Studies show that EoE can run in families so genetics may play a role in an individual’s susceptibility to the condition.
A study in The Journal of Allergy and Clinical Immunology found that individuals with a family history of EoE or other allergic diseases like asthma or eczema are more likely to develop the condition. But environmental risk factors especially food allergies are also big contributors.
Who is at Risk for Eosinophilic Esophagitis?
EoE can affect people of all ages, but certain groups are more at risk. These include:
Males
EoE is more common in men. Although the female ratio of approximately 3:1.
Individuals with Allergies
Those with a history of allergic conditions, such as asthma, eczema, or hay fever, are at a higher risk of developing EoE. People with atopic dermatitis, along with other allergic conditions, may have a higher risk of developing EoE.
Family History
As mentioned, having a family member with EoE or other allergic conditions increases the likelihood of developing the disease.
Young Children and Adults
While EoE can occur at any age, it is most commonly diagnosed in children and young adults.
Esophagitis Eosinophilic – Symptoms and Diagnosis
What are the Symptoms?
Symptoms of eosinophilic esophagitis can vary depending on age and the severity of the condition, and it is important to seek medical attention for severe or frequent symptoms. Common symptoms include:
Difficulty Swallowing (Dysphagia)
This is one of the most common symptoms, where individuals experience a sensation of food getting stuck or food getting stuck up in the esophagus.
Food Impaction
In severe cases, food can become lodged in the esophagus, requiring emergency medical intervention to remove it.
Chest Pain
Often mistaken for heartburn, chest pain, and stomach pain in EoE is related to esophageal inflammation.
Persistent Heartburn or Acid Reflux
Unlike typical acid reflux, these symptoms do not respond well to standard GERD treatments.
Abdominal Pain
Some individuals experience upper abdominal pain, particularly after eating.
Nausea and Vomiting: These symptoms are more common in children with EoE.
Failure to Thrive
In children, EoE can lead to poor weight gain or growth due to difficulty eating.
How Do Doctors Diagnose Eosinophilic Esophagitis?
Diagnosing EoE typically involves a combination of patient history, symptom assessment, and diagnostic tests. The following steps are commonly taken:
Patient History and Symptom Assessment:
The health care providers will review the patient’s medical history, focusing on symptoms related to trouble swallowing and any known allergies.
Upper Endoscopy
An essential diagnostic tool for EoE is an upper endoscopy (esophagogastroduodenoscopy or EGD). The doctor inserts a thin, flexible tube with a camera through the mouth to view the esophagus. The doctor looks for signs of inflammation, narrowing, or rings in the esophagus, which are indicative of EoE.
Biopsy
During the endoscopy, doctors take small tissue samples (biopsies) from the esophagus. These samples are then examined under a microscope to check for the presence of eosinophils. A high count of eosinophils in the esophageal tissue confirms the diagnosis of EoE.
Allergy Testing
Often related to food, seasonal allergies are. Thus, doctors recommend allergy testing to identify specific allergens that could be triggering the condition. This testing can include skin prick tests or blood tests.
Healthcare providers play a crucial role in diagnosing EoE, and their awareness and collaboration with researchers are essential for advancing knowledge and treatment options for this condition.
What Tests Are Used to Confirm?
In addition to the biopsy taken during an upper endoscopy. Doctors perform other tests to confirm EoE including:
Esophageal pH Monitoring
This test measures the amount of acid in the esophagus over 24 hours to distinguish between EoE and acid reflux.
Barium Swallow
To perform this imaging test, the patient swallows a barium solution that coats the esophagus, making it visible on X-rays. Similarly, this process can reveal narrowing or structural changes in the esophagus. It may indicate Eosinophilic Esophagitis (EoE).
What Happens if Eosinophilic Esophagitis is Left Untreated?
If left untreated, EoE can lead to several complications, including:
Esophageal Strictures
Chronic inflammation can cause the esophagus to narrow, leading to strictures that make swallowing difficult and increase the risk factor of food impaction.
Food Impaction
Frequent episodes of food becoming stuck in the esophagus can occur, sometimes requiring emergency and medical emergency intervention.
Malnutrition
Difficulty swallowing can lead to inadequate food intake, resulting in malnutrition, particularly in children.
Fibrosis
Long-term inflammation can cause scarring of the esophageal tissue, leading to permanent damage and loss of function.
Can it Cause Long-Term Problems?
Yes, if not managed properly EoE can cause long-term problems. Chronic inflammation and scarring can cause permanent narrowing of the esophagus making it hard to eat and swallow food. Untreated EoE can also cause quality-of-life issues such as chronic pain, anxiety about eating, and social difficulties related to food avoidance.
What is the Difference Between Eosinophilic Esophagitis and Gastroesophageal Reflux Disease?
EoE and GERD have similar symptoms such as heartburn and difficulty swallowing but they are different conditions. GERD is caused by acid reflux where stomach acid flows back into the esophagus and irritates it. EoE is an allergic reaction that causes eosinophils to accumulate in the esophagus.
Unlike GERD, EoE does not respond to acid-suppressing medications like PPIs. Doctors recommend a biopsy to differentiate between the two conditions as the presence of eosinophils in the esophagus confirms EoE. Additionally, there are online tools to calculate GERD stages that can help determine the symptoms score to understand the difference between Eosinophilic Esophagitis and Gastroesophageal Reflux Disease.
How is Eosinophilic Esophagitis Diagnosed in Children?
In children, diagnosing EoE can be tricky as symptoms often overlap with other common pediatric conditions like GERD or food allergies. In addition to the methods above, pediatricians may consider symptoms like failure to thrive, feeding and swallowing difficulties, and vomiting when evaluating a child for EoE. A pediatric gastroenterologist will do the endoscopy and biopsy for diagnosis.
Esophagitis Eosinophilic – Diet and Triggers
What Foods Trigger Eosinophilic Esophagitis?
Certain foods are known to trigger EoE in susceptible individuals. The most common food triggers include:
-
Dairy Products – Milk and other dairy products are among the most common triggers for EoE.
-
Wheat – Gluten-containing products can provoke an allergic response in some individuals with EoE.
-
Soy – Soy and soy-based products are another frequent trigger.
-
Eggs – Eggs are a known allergen that can trigger EoE symptoms.
-
Nuts: Both tree nuts and peanuts can cause allergic reactions in those with EoE.
-
Seafood – Fish and shellfish are potential triggers for EoE.
EoE is a type of eosinophilic gastrointestinal disease (EGID). In fact, organizations dedicated to supporting patients with these disorders play a significant role in providing resources and advancing research initiatives.
Identifying and avoiding these trigger foods is a critical part of managing EoE. Allergy testing and an elimination diet – often used to pinpoint specific food triggers.
What Are the Six Foods to Avoid?
The six foods most commonly eliminated in an EoE diet are:
-
Milk.
-
Wheat.
-
Soy.
-
Eggs.
-
Nuts (tree nuts and peanuts).
-
Seafood (fish and shellfish).
One effective approach is the “Six-Food Elimination Diet” (SFED). Particularly designed to remove the most common food allergens associated with EoE. After eliminating them, they gradually reintroduced one at a time while monitoring for symptoms to identify specific triggers.
How Does Diet Impact Eosinophilic Esophagitis?
Diet plays a central role in both the management and treatment of EoE. By identifying and eliminating trigger foods, many individuals with EoE can achieve symptom relief and reduce inflammation in the esophagus. Studies have shown that dietary management can be as effective as medication in controlling EoE symptoms.
A study published in the Journal of Pediatric Gastroenterology and Nutrition found that dietary elimination successfully induced remission in 75% of children with EoE.

Can Food Allergies Cause Eosinophilic Esophagitis?
Yes, food allergies are a primary cause of EoE. The condition is considered a form of food allergy-driven inflammation. Where certain foods trigger an immune response leading to the accumulation of blood cells called eosinophils, in the esophagus. Additionally, food allergy, testing, and dietary management are essential components of EoE treatment.
What is the Elimination Diet for Eosinophilic Esophagitis?
The elimination diet is a cornerstone of EoE management. It involves removing common food allergens from the diet and then systematically reintroducing them to identify specific triggers. There are different types of elimination diets used in EoE, including:
Six-Food Elimination Diet (SFED)
This diet eliminates the six most common food allergens (milk, wheat, soy, eggs, nuts, and seafood).
Four-Food Elimination Diet
This more restricted version eliminates four major allergens (milk, wheat, soy, and eggs).
Elemental Diet
In severe cases, an elemental diet is used, where all foods are replaced with an amino acid-based formula that is hypoallergenic.
Once symptoms improve, foods are gradually reintroduced under medical supervision to determine which specific foods are triggering the condition.
Are There Any Safe Foods?
Safe foods vary depending on the individual’s specific food triggers, but generally, common foods that are less likely to cause allergic reactions include:
-
Fruits – Most fresh fruits are safe, except citrus fruits for some individuals.
-
Vegetables – Non-starchy vegetables like leafy greens, cucumbers, and carrots are typically safe.
-
Rice and Quinoa – These grains are usually well-tolerated.
-
Meats: Non-processed meats like chicken, turkey, and lamb are often safe options.
It’s essential to work with a healthcare provider or dietitian to develop a personalized safe food list.
How to Reintroduce Foods After an Elimination Diet for EoE?
Reintroducing foods happens gradually and under medical supervision. Typically, one food is reintroduced at a time over several weeks. The medical team monitored the patient for any recurrence of symptoms. If symptoms return, then doctors recommend eliminating it again. This process helps identify specific food triggers while maintaining a balanced diet.

Esophagitis Eosinophilic – Treatment Options
Can You Cure Eosinophilic Esophagitis?
Currently, there is no cure for EoE. Eventually managed through a combination of dietary changes, medications, and lifestyle modifications. The goal of treatment for chronic disease is to reduce symptoms, heal the esophagus, and prevent complications such as strictures. With proper management, individuals with EoE can lead healthy, active lives.
What Are the Treatment Options?
Treatment for EoE typically involves a multi-faceted approach that includes:
Dietary Management
The elimination diet, as described earlier, is often the first line of treatment for EoE. Identifying and avoiding trigger foods can significantly reduce symptoms. Nonprofit organizations and research consortia, such as the American Partnership for Eosinophilic Disorders and the Consortium of Eosinophilic Gastrointestinal Disease Researchers (CEGIR), play a crucial role in providing resources and support for individuals and families affected by eosinophilic gastrointestinal disorders.
Medications
Often medications combined with dietary changes to control inflammation and prevent symptoms. Common medications include:
-
Proton Pump Inhibitors (PPIs) – Although traditionally used for acid reflux, PPIs can reduce esophageal inflammation in some people with EoE.
-
Topical Steroids – Swallowed corticosteroids, such as fluticasone or budesonide. To reduce inflammation in the esophagus. Typically taken in a liquid or inhaler form (without inhaling) and swallowed to coat the esophagus.
-
Biologic Therapies – Emerging treatments like dupilumab, a monoclonal antibody that targets specific immune pathways involved in EoE, are showing promise in clinical trials.
Esophageal Dilation
If strictures have developed, esophageal dilation may be necessary. This procedure stretches the narrowed parts of the esophagus to make swallowing easier. But it doesn’t treat the underlying inflammation. Usually considered when other treatments have failed.
Allergy Management
If your EoE is related to environmental allergies or allergens. The doctors recommend allergy treatments like antihistamines or allergen immunotherapy (allergy shots).
How Well Do Medications Work?
Medications can be very effective for EoE especially when dietary changes alone aren’t enough. Proton pump inhibitors (PPIs) temporarily reduce esophageal inflammation in some patients with EoE even when acid reflux isn’t present.
According to a 2023 study in Gastroenterology, topical steroids like fluticasone and budesonide work in reducing eosinophils in the esophagus and symptoms in up to 70% of patients.
These medications reduce inflammation and prevent the eosinophils from accumulating in the esophagus. But medications aren’t a permanent cure for EoE. In some cases, patients have to take them for a long term to manage the condition. And while medications can control symptoms and inflammation, they don’t address the underlying allergic triggers of EoE which is why dietary management is still a big part of the treatment plan.
What Lifestyle Changes Can Help Manage?
In addition to dietary management and medications, certain lifestyle changes can help manage EoE and improve quality of life. These include:
Eating Smaller, More Frequent Meals
This can help prevent food from becoming stuck in the esophagus and reduce other symptoms because of dysphagia.
Chewing Food Thoroughly
Ensuring to chew food thoroughly before swallowing can reduce the risk of food impaction and improve the digestive system.
Avoiding Late-Night Eating
Eating late at night can exacerbate symptoms, particularly if lying down shortly after you stop eating.
Elevating the Head of the Bed
For individuals who experience heartburn or acid reflux in addition to EoE, elevating the head of the bed can help reduce symptoms and manage related problems.
Managing Stress
Stress can exacerbate EoE symptoms in some individuals. Techniques such as mindfulness, meditation, and regular exercise can help manage stress levels.

What Do Steroids Do in Eosinophilic Esophagitis?
Steroids are key in EoE treatment by reducing inflammation caused by the accumulation of esophagus eosinophils and preventing further eosinophil buildup in the esophagus. For treating EoE, doctors usually use topical steroids, such as fluticasone and budesonide. These steroids come in a form that coats the esophagus, allowing the medication to target the affected area directly. Unlike inhaled steroids, they are swallowed, effectively reducing symptoms and esophageal inflammation in many EoE patients.
According to a study in the Journal of Allergy and Clinical Immunology, topical steroids can achieve histologic remission (eosinophil counts back to normal) in up to 50-60% of patients. Generally well tolerated with fewer systemic side effects than oral steroids, consistency is key, although some patients may need long-term therapy.
Can it be Managed Without Medications?
For some, EoE can manage without medication. Especially if dietary changes are enough to control symptoms. Subsequently, the elimination diet therapy as described above is often the first line of treatment. If dietary management alone is successful, then doctors may not prescribe medications.
However, not all patients respond to dietary changes. Then it is essential to take meds. Not only to control symptoms but also to prevent complications. Regardless, EoE patients should work with their doctor to figure out what’s best for them.
Are There New Treatments?
In the past decade, the research has been ongoing for new EoE treatments and several are in the works. One of the most promising is biologic therapy which targets the immune pathways involved in the allergic response. Dupilumab, a monoclonal antibody that blocks certain cytokines involved in EoE, is looking good in trials and maybe a new option for moderate to severe EoE patients.
Other new treatments include new meds that target eosinophils directly and new formulations of existing meds that may be more effective or have fewer side effects. Research into the underlying causes of EoE is also ongoing to develop more targeted and better treatments in the future.
Nonetheless, eosinophilic esophagitis is a complex chronic condition that requires management through a combination of diet, meds, and lifestyle changes. There is no cure for EoE but research and new treatments offer hope for better outcomes and quality of life for those with the condition.
Always consult with a healthcare professional for personal medical advice and treatment options.











