Gastric Sleeve 10-Year Post-Surgery
Gastric sleeve 10 years post-surgery is an important topic for patients considering or who have undergone the gastric sleeve procedure. Subsequnetly understanding the crucial aspects of post-gastric sleeve surgery and recognizing the signs of malnutrition is equally important. Consequently, helps them understand the long-term outcomes for more informed decision-making and ongoing care.
Physical Changes
Firstly, let’s explore the physical changes that typically occur throughout a 10-year post-surgery. Following gastric sleeve surgery, patients often experience significant weight loss in the initial months and years. This weight reduction stems from the surgery’s effect of reducing stomach capacity, leading to decreased food intake and calorie absorption. Maintaining weight loss in the long term requires sustained lifestyle modifications, including dietary adjustments and regular exercise.
While many patients successfully maintain their weight loss, some may face challenges with weight regain over time. This highlights the importance of continued support, monitoring, and adherence to healthy habits. In addition to weight loss, gastric sleeve surgery can improve or resolve obesity-related health conditions such as type 2 diabetes, high blood pressure, and sleep apnea. These improvements can significantly enhance patients’ long-term health and quality of life.
However, it’s important to recognize that gastric surgery is not a quick fix. In the end, this is still just a tool. While surgery can facilitate weight loss and improve metabolic health, it’s not a substitute for a comprehensive lifestyle change. Patients must remain committed to healthy eating habits, portion control, and physical activity to optimize their long-term outcomes. Furthermore, gastric sleeve surgery carries potential risks and complications, although they are relatively rare.
These complications include gastric leaks, strictures, and nutritional deficiencies, which emphasize the importance of regular follow-up appointments and adherence to post-operative guidelines.
Psychological Changes
From a psychological standpoint, the journey after a gastric sleeve surgery can be both rewarding and challenging. Patients may experience fluctuations in mood, body image concerns, and difficulties adjusting to new eating patterns.
It’s essential for patients to receive ongoing support from healthcare professional support groups and loved ones to navigate these emotional complexities effectively. In summary, a decade after gastric sleeve surgery, patients may experience significant physical, metabolic, and psychological changes.
While the procedures can be life-changing, they require dedication to healthy habits, ongoing monitoring, and support from healthcare providers and loved ones. By embracing these principles, patients can optimize their long-term health and well-being after gastric sleeve surgery.
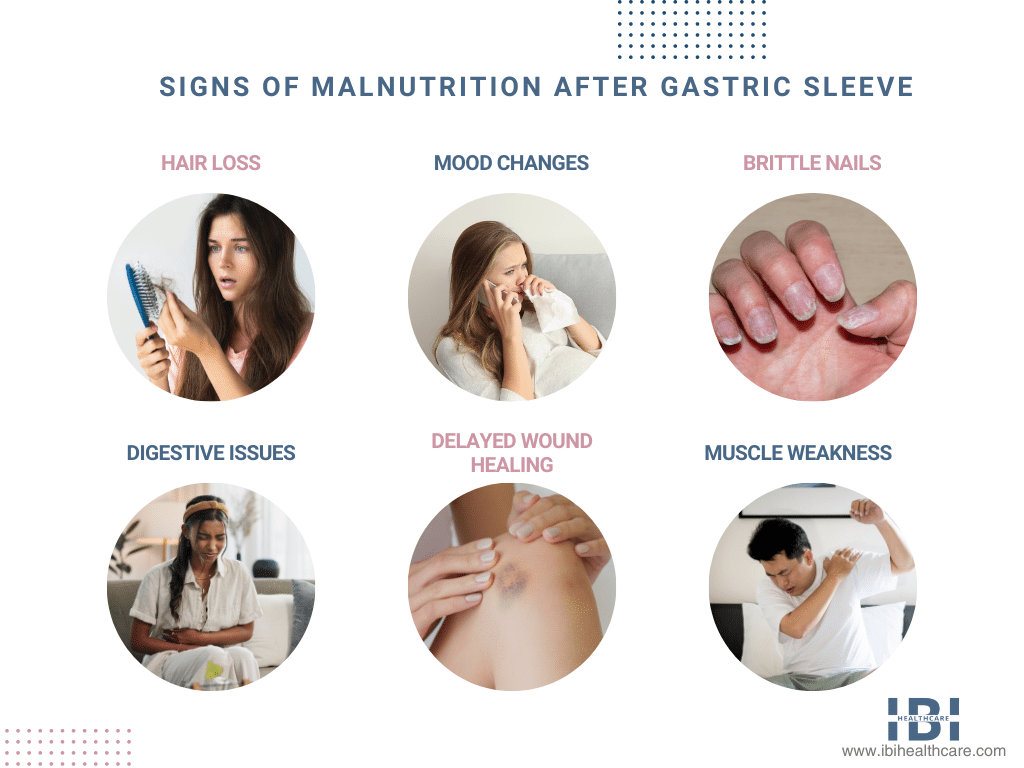
Gastric Sleeve 10-Year Post-Surgery – Signs of Malnutrition
While gastric sleeve procedure can bring about remarkable weight loss and health improvement, it does have risks which include the potential for malnutrition in patients. Understanding signs is vital for both the patient and healthcare providers to ensure long-term health and well-being.
- One of the primary signs of malnutrition after gastric sleeve surgery is unexplained weight loss. While shedding excess weight is expected, rapid or excessive weight loss beyond what is considered healthy could indicate underlying nutritional deficiencies.
- Fatigue, weakness, and decreased energy levels are common symptoms of malnutrition. When the body lacks essential nutrients, it struggles to function optimally leading to these feelings of tiredness and lethargy.
- Changes in skin, hair, and nails can also signal malnutrition. Patients may notice hair thinning, dry skin, and brittle nails, all of which can be indicative of deficiencies in vital nutrition like protein, vitamins, and minerals.
- Gastrointestinal symptoms such as nausea, vomiting, diarrhea, and abdominal pain may occur. These symptoms can disrupt nutrient absorption and exhaust away existing deficiencies. not addressed promptly.
- Mood strains, irritability, and cognitive impairment may also manifest as signs of malnutrition. Nutrient deficiencies can impact brain health and neurotransmitter functions, affecting mood and cognitive function.
- Specific nutrient deficiencies such as vitamin B12, iron, calcium, and vitamin D deficiencies can cause unique symptoms like numbness and tingling in the extremities, muscle weakness, bone pain, and increased stability to fractures.
Meet Dr. Jenn Huang – Gastric Sleeve Surgeon
Dr. Jenny Huang at IBI Healthcare Institute is a bariatric surgeon, who specializes in weight loss surgery and medication. I recommend bariatric patients recognize signs of malnutrition after gastric sleeve surgery as early as possible. Staying proactive in monitoring nutritional status through blood tests and nutritional assessments is equally crucial. Bariatric surgeons can help in identifying and addressing signs of malnutrition through personalized dietary counseling, supplementation, and medical intervention when necessary.
Additionally, patients should follow the bariatric surgeon’s post-operative instructions, and report any concerning symptoms promptly. With proper care and monitoring, patients can minimize the risk of complications. Lastly, achieve successful long-term weight loss and improved health outcomes.











