Hyperglycemia Overview
Hyperglycemia, high blood sugar, is a condition often linked to diabetes mellitus, which is a critical factor in differentiating between types of hyperglycemia. However, it’s important to note that hyperglycemia can occur in nondiabetics as well. This occurs when there’s too much glucose in the blood. If left unchecked hyperglycemia can cause severe health complications so it’s important to know its symptoms, causes, and management.
Is Hyperglycemia a Diabetic Disease?
Hyperglycemia is commonly associated with diabetes but it’s not a diabetic disease. Diabetes is a chronic disease where the body either doesn’t produce enough insulin or doesn’t use it properly. Hyperglycemia can occur in both diabetic and nondiabetic individuals.
In diabetics, hyperglycemia occurs when blood sugar levels rise due to a lack of insulin or ineffective use of insulin. In non-diabetics, hyperglycemia can occur when blood sugar rises due to other factors such as stress, illness, or certain medications. Differentiating between types of hyperglycemia is crucial, particularly in understanding the role of diabetes mellitus, which involves insulin resistance and can lead to cognitive decline.
Is Hyperglycemia the Same as Diabetes?
No, hyperglycemia and diabetes are not the same. Diabetes is a chronic condition where the body has difficulty regulating blood sugar levels effectively, either due to insufficient insulin production (Type 1 diabetes) or the body’s inability to use insulin properly (Type 2 diabetes). Furthermore, this imbalance can lead to various health complications if not managed properly.
Additionally, hyperglycemia is a symptom or condition where blood glucose levels are too high. Besides this, hyperglycemia is a characteristic of diabetes but can also be a temporary condition in non-diabetics. Especially during illness, stress, or as a side effect of medications like corticosteroids.
What Causes Hyperglycemia?
Risk factors for hyperglycemia include specific medical conditions such as obesity and pancreatitis, medications like steroids, and demographic factors such as age and ethnicity. Here are some common causes and symptoms of hyperglycemia especially for those with diabetes:
Missing or Not Taking Enough Insulin
If you’re on insulin, missing a dose or not taking enough insulin can cause your blood sugar to go up.
Eating Too Many Carbs
Consuming more carbs than your body can process can cause high blood sugar.
Lack of Physical Activity
Exercise helps your body use glucose for energy. However, without enough physical activity, glucose stays in your bloodstream and causes hyperglycemia.
Illness or Infection
Your body releases stress hormones to fight illness which can raise your blood sugar.
Stress
Physical or emotional stress can cause hyperglycemia by releasing stress hormones like cortisol and adrenaline.
Medications
Certain medications like steroids can cause blood sugar to spike.
Can Stress Cause Hyperglycemia?
Yes, stress can cause hyperglycemia.
When you’re stressed, your body releases hormones like cortisol and adrenaline. These hormones can cause your blood sugar levels to rise, which can be particularly challenging for individuals with diabetes to manage. This is part of your body’s natural “fight or flight” mechanism to respond to a perceived threat.
But for those with diabetes or prone to high blood sugar, this response can cause hyperglycemia. Specially, for those with diabetes, need to recognize stress as a trigger and manage it well.
How Does Hyperglycemia Occur in Non-Diabetics?
In non-diabetics, hyperglycemia can occur for many reasons. For example, when we are under extreme stress the body will produce more glucose to fuel the “fight or flight” response. Illness or infection can also cause temporary hyperglycemia as the body releases hormones to fight the illness and inadvertently raises blood sugar levels.
Certain medications like steroids can also cause temporary spikes in blood sugar. Although they are not diabetic, they can still get hyperglycemia called high blood sugar under certain circumstances.
What Are The Triggers for Hyperglycemia in Diabetics?
In diabetics, the following can cause hyperglycemia:
Poor Diet
Eating foods high in carbs or sugar can raise blood sugar levels.
Skipping Medications
Missing insulin or other diabetes meds can cause blood sugar to rise.
Physical Inactivity
Not exercising can prevent the body from using glucose.
Stress
Both physical and emotional stress can raise blood sugar levels.
Illness or Infection
The body’s response to illness can cause blood sugar to rise.
Hormonal Changes
In women, hormonal changes during menstruation or pregnancy can affect blood sugar.
Lack of Sleep
Not sleeping can increase stress and disrupt glucose metabolism.

Hyperglycemia – Symptoms and Signs
Knowing the symptoms of hyperglycemia is key to managing the condition and preventing complications. Early detection means you can intervene before it gets worse.
What Are the Symptoms of Hyperglycemia?
The symptoms of hyperglycemia can vary depending on severity and duration. Here are the common ones:
Thirst
One of the first signs of hyperglycemia is thirst, as the body tries to flush out excess glucose through urine.
Frequent Urination
High blood sugar levels compel the kidneys to work harder to filter and absorb the excess glucose. This increased workload can lead to frequent urination, as the body attempts to expel the surplus sugar through urine.
Fatigue
When the body can’t use glucose for energy, it can lead to extreme tiredness.
Blurred Vision
High blood sugar levels can cause the lenses in the eyes to swell, resulting in blurred vision.
Headaches
Persistent high and low blood sugar levels can cause headaches.
Dry Mouth and Skin
Dehydration from frequent urination can cause dry mouth and skin.
What Are the 3 Signs of Hyperglycemia?
The three most common signs or symptoms of hyperglycemia include:
- Increased Thirst – The body tries to compensate for high blood sugar levels by increasing fluid intake.
- Frequent Urination – The kidneys work overtime to expel excess glucose through urine, leading to frequent trips to the bathroom.
- Fatigue – The inability to use glucose for energy leads to persistent tiredness.
How Do Early Signs of Hyperglycemia Differ from Advanced Symptoms?
Early signs of hyperglycemia, such as increased thirst and frequent urination, are often mild and can be easily overlooked. However, if left untreated, hyperglycemia can lead to more severe symptoms such as:
Ketoacidosis
A serious condition where the body starts breaking down fat for energy, leading to the production of ketones, which can build up in the bloodstream and become toxic.
Unexplained Weight Loss
The body starts to break down muscle and fat for a primary source of energy when it cannot use glucose effectively.
Nausea and Vomiting
As ketones build up in the bloodstream, they can cause nausea and vomiting.
Confusion or Difficulty Concentrating
Severe hyperglycemia can affect cognitive function, leading to confusion or difficulty concentrating.
Can Hyperglycemia Occur Without Noticeable Symptoms?
Yes, hyperglycemia can occur without noticeable symptoms, especially in its early stages. Hyperglycemia diagnosed typically involves a review of medical history, physical examinations, and various blood tests, including fasting blood glucose, hemoglobin A1C, and an oral glucose tolerance test or tests. Some people may not experience the classic symptoms of increased thirst, frequent urination, or fatigue.
This is why regular monitoring of blood sugar levels is essential, particularly for individuals with diabetes or those at risk of developing hyperglycemia. Silent hyperglycemia can lead to serious long-term complications if not detected and managed promptly.
How Does Hyperglycemia Affect the Body Long-Term?
Over time, uncontrolled hyperglycemia can lead to severe complications. Chronic high blood sugar and high blood glucose levels can damage blood vessels, nerves, and organs throughout the body. Some of the long-term effects of chronic hyperglycemia include:
Cardiovascular Disease
Hyperglycemia can increase the risk of heart disease, stroke, and other cardiovascular complications.
According to the American Diabetes Association (ADA), individuals with diabetes are two to four times more likely to die from heart disease compared to those without diabetes.
Nerve Damage (Neuropathy)
Prolonged high blood sugar can damage the nerves, particularly in the legs and feet, leading to numbness, pain, and potential loss of sensation.
The Centers for Disease Control and Prevention (CDC) notes that 50% of people who have diabetes or with diabetes develop some form of neuropathy.
Kidney Damage (Nephropathy)
Hyperglycemia can cause the kidneys to filter too much blood, which over time, can lead to kidney damage and eventually kidney failure.
Diabetic nephropathy is a leading cause of kidney failure in the United States, affecting about 25% of individuals with diabetes, according to the National Kidney Foundation.
Eye Damage (Retinopathy)
High blood sugar can damage the blood vessels in the eyes, leading to conditions like diabetic retinopathy, which can result in blindness.
The World Health Organization (WHO) reports that diabetic retinopathy is the leading cause of vision loss in working-age adults.
Foot Problems
Nerve damage and poor blood flow due to hyperglycemia can lead to severe foot infections and ulcers, which in extreme cases, may require amputation.
The International Diabetes Federation (IDF) estimates that up to 15% of people with diabetes will develop a foot ulcer in their lifetime.
Skin Conditions
High blood sugar levels can make individuals more susceptible to skin infections and conditions like diabetic dermopathy.

Managing Hyperglycemia
Managing hyperglycemia effectively is crucial to prevent the complications mentioned above. This involves a combination of lifestyle changes, medication, and regular monitoring.
How to Deal with Hyperglycemia?
Dealing with hyperglycemia involves taking immediate steps to lower blood sugar levels and prevent them from rising too high in the future. Some strategies include:
Taking Prescribed Medication
Ensure that you take insulin or oral diabetes medications as prescribed by your healthcare provider.
Monitoring Blood Sugar Levels
Regular monitoring can help you catch hyperglycemia early and take corrective actions.
Staying Hydrated
Drinking water can help flush excess glucose out of the bloodstream.
Adjusting Diet
Reduce your intake of carbohydrates and sugars to prevent further spikes in blood sugar.
Exercising
Physical activity helps lower blood sugar levels by using glucose for energy.
What to Do if Someone Has a Hyperglycemic Episode?
If someone is experiencing a hyperglycemic episode, it’s important to act quickly. Here are the steps to take:
Check Blood Sugar Levels
Use a glucose meter to confirm that blood sugar levels are high.
Administer Insulin
If the person uses insulin, they may need a dose to bring their blood sugar levels down. Follow the prescribed insulin regimen.
Drink Water
Encourage the person to drink water to help flush out excess glucose.
Seek Medical Help
If blood sugar levels remain high despite taking corrective measures, or if the person becomes confused, drowsy, or exhibits symptoms of diabetic ketoacidosis (DKA), seek emergency medical attention immediately.
What to Do if a Patient is Hyperglycemic?
If a patient in a clinical setting is hyperglycemic, we take action right away. Here’s a quick guide for healthcare providers:
Check Blood Glucose
Use a glucose meter to get the current blood sugar reading. Document and compare to previous readings to see trends.
Review Medications
Review the patient’s insulin or oral meds. If on insulin, check the dose and timing to make sure they’re getting the right amount.
Take Insulin
If blood sugar is way high, give a corrective dose of insulin according to the patient’s sliding scale or insulin protocol. Make sure the dose is right for the level of hyperglycemia.
Hydrate
Encourage or give fluids (water) to help the body get rid of excess glucose. If the patient can’t drink, consider intravenous fluids if appropriate.
Watch for Complications
Look for signs of diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS), which are serious complications of untreated hyperglycemia. Symptoms include nausea, vomiting, abdominal pain, fruity breath odor, rapid breathing, confusion or unconsciousness.
Adjust Plan
Review diet, exercise, and meds. May need to make changes to prevent future hyperglycemic episodes. This might be diet counseling, med changes, or activity changes.
Educate the Patient
Once the acute episode is managed, take the time to educate the patient on how to recognize early signs of hyperglycemia, the importance of medication adherence, and lifestyle changes.
Follow-up
Schedule a follow-up or check-in to check blood sugar and overall health. Follow-ups are key to the long-term management of hyperglycemia.

What is the Treatment for Hyperglycemia?
The first line of treatment for hyperglycemia is lifestyle changes (diet and exercise) and meds. Hyperglycemia treated varies based on its underlying causes, with medical emergencies like DKA and HHS requiring immediate treatment with intravenous fluids, electrolytes, and insulin. For type 1 diabetes insulin is the first line of treatment. For type 2 diabetes metformin is often the first oral hypoglycemic agent. If blood sugar is not controlled additional meds or insulin may be added.
Insulin Therapy
For type 1 diabetics, insulin is crucial for managing blood sugar. It’s also used in type 2 diabetes when other medications aren’t sufficient. Insulin helps lower the blood glucose level by enabling cells to absorb sugar from the bloodstream.
Oral Medications
For type 2 diabetes, medications like metformin help the body use insulin more effectively. Other drugs, such as sulfonylureas, increase insulin production, while SGLT2 inhibitors help eliminate glucose through urine.
Lifestyle Modifications
Alongside medications, diet, and exercise are critical. A balanced diet low in refined sugars and high in fiber can help control blood sugar levels. Regular physical activity helps the body use glucose efficiently and lowers blood sugar levels.
How Can Diet and Exercise Help Manage Hyperglycemia?
Diet and exercise are foundational in managing diabetes and hyperglycemia. Here’s how they help:
Diet:
- Low-Carb Diet – Reducing carbohydrate intake can prevent spikes in blood sugar levels. Choose whole grains over refined grains and opt for non-starchy vegetables, lean proteins, and healthy fats.
- Glycemic Index – Eating foods with a low glycemic index (GI) can help manage blood sugar levels. Foods like oats, legumes, and non-starchy vegetables have a low GI and cause slower, more controlled rises in blood sugar.
- Regular Meals – Eating at regular intervals helps maintain stable blood sugar levels. Skipping meals can lead to fluctuations in blood sugar, increasing the risk of hyperglycemia.
Exercise:
- Increased Glucose Utilization – Physical activity increases the body’s sensitivity to insulin and helps cells absorb glucose for energy. Even moderate exercise, like walking, can significantly lower blood sugar levels.
- Weight Management – Exercise helps with weight management, which is crucial for individuals with type 2 diabetes. Excess weight can worsen insulin resistance, leading to higher blood sugar levels.
- Stress Reduction – Regular exercise can reduce stress levels, which in turn can help prevent stress-induced hyperglycemia
What Medications Are Commonly Used to Treat Hyperglycemia?
Several medications are used to treat hyperglycemia, particularly in individuals with diabetes. These include:
Insulin
As mentioned, insulin is the primary treatment for type 1 diabetes and is also used in type 2 diabetes when other treatments fail. It comes in various forms, including rapid-acting, short-acting, intermediate-acting, and long-acting.
Metformin
Often the first medication prescribed for type 2 diabetes, metformin helps lower glucose production in the liver and improves the body’s sensitivity to insulin.
Sulfonylureas
These medications stimulate the pancreas to produce more insulin. Examples include glipizide and glyburide.
DPP-4 Inhibitors
These drugs help lower blood sugar levels by preventing the breakdown of a hormone that increases insulin release after meals.
SGLT2 Inhibitors
These drugs help the kidneys remove glucose from the bloodstream through urine. Examples include canagliflozin and dapagliflozin.
GLP-1 Receptor Agonists
These medications increase insulin production and decrease glucose production by the liver. They also slow down digestion, which helps control blood sugar levels.
How Can You Prevent Hyperglycemia in Diabetes?
Preventing hyperglycemia requires a proactive approach that includes lifestyle changes, regular monitoring, and adherence to treatment plans. Here are some strategies:
Regular Monitoring
Frequent blood sugar checks can help catch hyperglycemia early. Use a glucose meter or continuous glucose monitor (CGM) to further keep track of your blood glucose levels.
Medication Adherence
Take your medications as prescribed. Set reminders if necessary to ensure you don’t miss a dose.
Healthy Diet
Follow a balanced diet that’s low in simple sugars and high in fiber. Certainly, meal planning can help you maintain steady blood sugar levels throughout the day.
Exercise Regularly
Engage in regular physical activity, aiming for at least 150 minutes of moderate exercise per week. Consequently, this helps improve insulin sensitivity and lowers blood sugar.
Stress Management
Practice stress-reduction techniques such as deep breathing, meditation, or yoga to prevent stress-induced hyperglycemia.
Regular Medical Check-ups
Visit your healthcare provider regularly for check-ups and lab tests to monitor your overall health.
What to Put in a Hyperglycemia Emergency Kit?
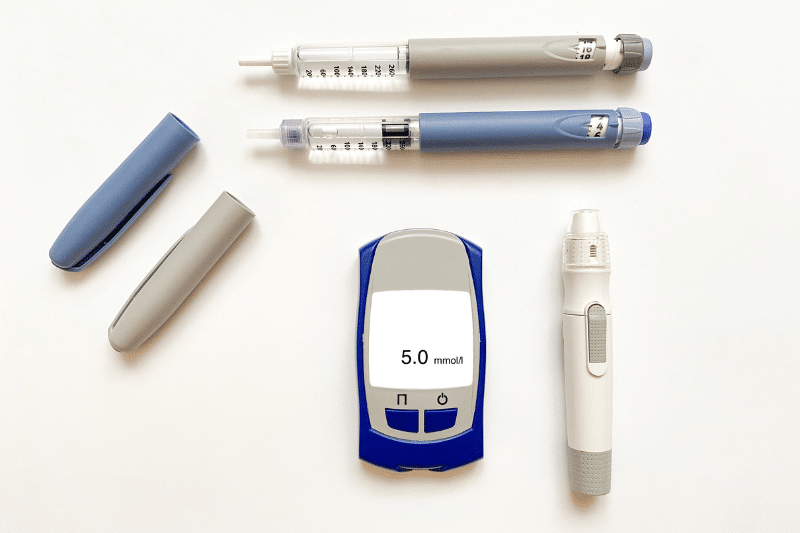
A hyperglycemia emergency kit is a must-have for both people who have diabetes and those with diabetes. Subsequently, it allows them to act fast if their blood sugar levels go too high. Here’s what to include:
- Glucose Meter and Test Strips – To test blood sugar levels fast.
- Insulin and Syringes/Pens – Fast-acting insulin to bring down high blood sugar.
- Glucagon Kit – While glucagon is used for lows, it’s good to have it on hand in case of severe lows after a high.
- Ketone Strips – To test for ketones in urine if blood sugar is above 240 mg/dL.
- Fast-acting Carbs – If blood sugar drops after insulin (e.g., glucose tablets, juice).
- Medical Information – List of medications, doses, and emergency contacts.
- Instructions – Clear instructions on how to manage hyperglycemia and when to get medical help.

Hyperglycemia – Complications and Risk Factors
If left unattended, hyperglycemia can be serious and even life-threatening.
What Are the Complications of Untreated Hyperglycemia?
Untreated hyperglycemia can cause:
Diabetic Ketoacidosis (DKA)
A serious condition where the body starts breaking down fat for energy and ketones build up. DKA is more common in type 1 but can occur in type 2 as well.
Hyperosmolar Hyperglycemic State (HHS)
A severe complication of hyperglycemia is seen in type 2 diabetes. When blood sugar gets extremely high, it causes severe dehydration and altered mental status. Regardless, HHS is life-threatening and needs immediate medical attention.
Chronic Complications
These are cardiovascular disease, neuropathy, nephropathy, retinopathy, and foot problems, as mentioned earlier.
How Does Hyperglycemia Cause Diabetic Ketoacidosis?
Diabetic ketoacidosis (DKA) occurs when the body starts breaking down fat for energy instead of glucose. This happens when insulin levels are too low and glucose can’t get into the cells. As a result, the body breaks down fat, it produces ketones which are acidic byproducts.
As a matter of fact, high levels of ketones cause acidosis where the blood becomes too acidic. Similarly, DKA has symptoms of nausea, vomiting, abdominal pain, fruity-smelling breath, and rapid breathing. Conversely, if left untreated, DKA can lead to coma or death.
What is the Difference Between Hyperglycemia and Hyperosmolar Hyperglycemic State (HHS)?
Both hyperglycemia and hyperosmolar hyperglycemic state (HHS) involve very high blood sugar, levels, but they differ in severity and symptoms:
Hyperglycemia
This refers to any blood sugar level above the normal range, typically above 180 mg/dL after meals or 130 mg/dL while fasting. Symptoms may include increased thirst, frequent urination, and fatigue.
Hyperosmolar Hyperglycemic State (HHS)
In fact, HHS is a more severe form of hyperglycemia, usually occurring in type 2 diabetes. Furthermore, it involves extremely high blood sugar levels, often above 600 mg/dL. Unlike DKA, there is little to no ketone production, so acidosis is less of a concern. However, HHS leads to severe dehydration and can cause confusion, seizures, or coma.

Hyperglycemic – Monitoring and Prevention
Effective monitoring and prevention strategies are essential in managing hyperglycemia and preventing diabetes complications too.
How Often Should I Check My Blood Sugar to Avoid Hyperglycemia?
The frequency of blood sugar checks depends on your diabetes management and diabetes meal plan. However, here are some general guidelines for blood sugar regularly:
Type 1 Diabetes
Check your blood sugar at least 4 times a day, before meals and before bed. More checks may be needed during exercise, illness, or changes in your routine.
Type 2 Diabetes
If on insulin, check your blood sugar at least 2 times a day. Although, if managed with oral meds or lifestyle changes. Then the frequency may vary. Nevertheless, your doctor will guide you based on your individual needs.
Continuous Glucose Monitoring (CGM)
CGM devices give you real-time blood sugar readings to catch hyperglycemia high blood before it gets severe. In addition, CGMs are great for people who have frequent serious blood pressure or sugar fluctuations.
How to Prevent Hyperglycemia?
Preventing hyperglycemia means making lifestyle changes:
Dietary Changes
Eat a balanced diet with portion-controlled carbs. Avoid sugary snacks and drinks. Instead have whole grains, lean proteins, and plenty of veggies.
Regular Exercise
Exercise regularly, at least 150 minutes of moderate exercise a week. Evidently, this improves insulin sensitivity and prevents blood sugar spikes.
Weight Management
Being at a healthy weight reduces insulin resistance, especially in type 2 diabetes.
Stress Management
Chronic stress raises blood sugar levels. Moreover, add stress-reducing activities like yoga, meditation, or hobbies to your daily routine.
Regular Check-ups
Keep up with your regular check-ups to monitor your overall health and make any necessary adjustments to your diabetes management plan.
How Does Continuous Glucose Monitoring (CGM) Help in Managing Hyperglycemia?
Indeed, continuous glucose monitoring (CGM) devices significantly contributed to diabetes management. Moreover, these devices give you real-time glucose readings so you can make informed decisions about your diet, exercise, and medication.
CGMs can detect rising blood sugar levels before they become a problem and allow for timely interventions. They also track trends in fasting blood glucose levels, and patterns in blood sugar fluctuations so healthcare providers can tailor their treatment plans better.
Firstly, understanding hyperglycemia, its causes, symptoms, and management is key for people with diabetes and those at risk. Secondly, by being proactive with monitoring, lifestyle changes, and proper medication. Eventually, hyperglycemia can be managed as well, and the risk of complications is reduced. Nonetheless, always consult with a healthcare provider for personalized advice and treatment plans.










