Prostate cancer disease is a big deal for men worldwide, including in the US. Knowing the symptoms, detection methods and treatment options is key to early intervention and management. In this guide, we will cover all aspects of prostate cancer, with the latest statistics, expert advice, and practical tips to help you make informed decisions about your health. Learn about common signs and when to seek medical advice for better outcomes.
What is Prostate Cancer Disease?
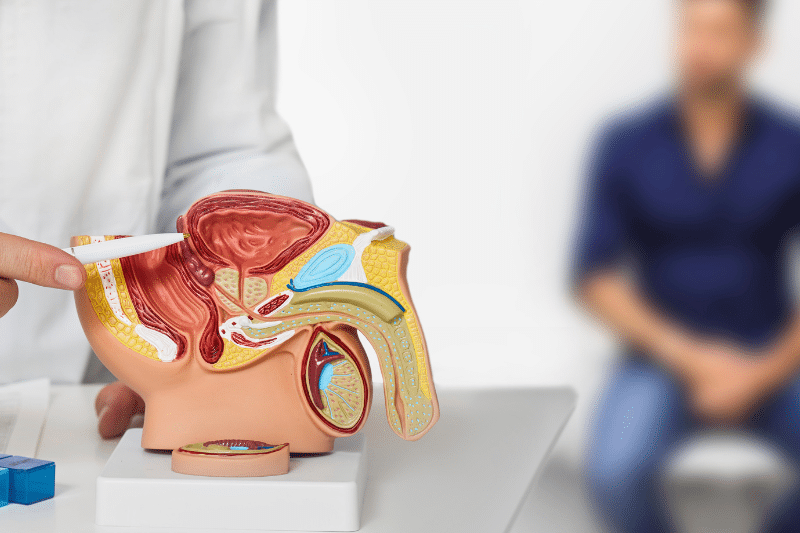
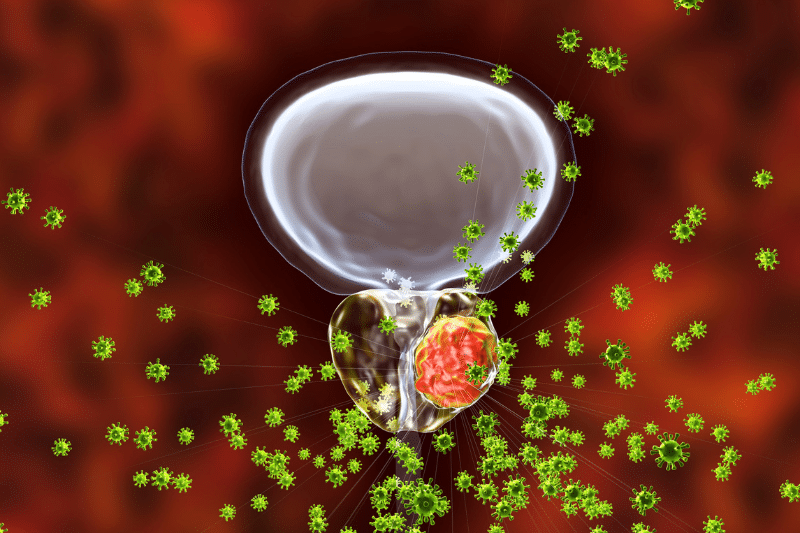
Prostate cancer originates in the prostate gland, a small, walnut-sized organ in men responsible for producing seminal fluid. Furthermore, prostate cancer begins when cells in the prostate mutate and develop changes in their DNA, leading to uncontrolled growth. Indeed, it ranks as one of the most frequently occurring cancers among men.
The American Cancer Society reports that 1 in 8 men will receive a diagnosis of prostate cancer at some point in their lives. On a global scale, it represents 3.8% of all cancer cases. Thus, the high incidence of prostate cancer underscores the importance of addressing and understanding this condition.
Prostate Cancer Disease – Symptoms and Early Detection
Early Signs and Symptoms
Early detection is key to successful treatment. However early-stage prostate cancer often has no symptoms. As prostate cancer develops and progresses symptoms may include:
-
Frequent urination especially at night.
-
Difficulty starting or stopping urination.
-
Weak or interrupted urine flow.
-
Pain or burning during urination.
-
Blood in urine or semen.
-
Pain in the lower back, hips, or thighs.
These symptoms can also be caused by cancer cells or other conditions so see a healthcare professional for a proper diagnosis.
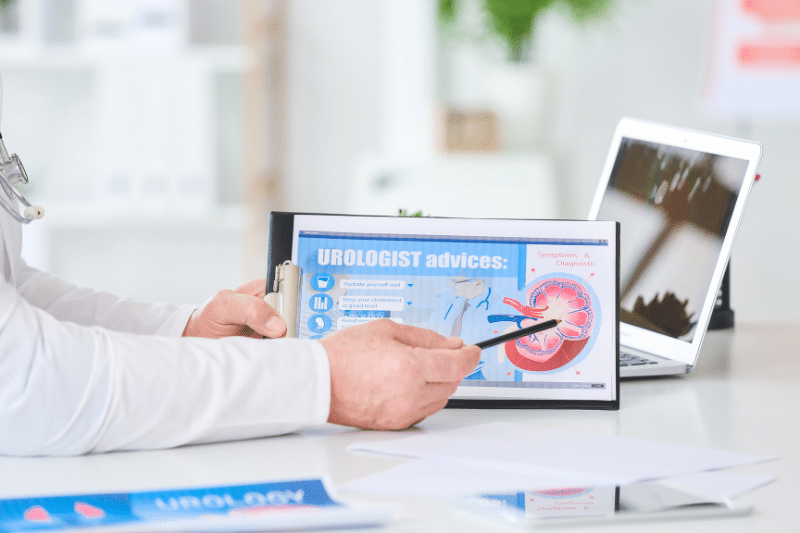
Detection Methods and Tests
As a matter of fact, early detection can make a big difference in treatment outcomes. Here are the methods and tests:
-
Prostate-Specific Antigen (PSA) Test – This blood test evaluates the level of PSA, a protein secreted by the prostate gland. High PSA levels may indicate prostate cancer, although other prostate conditions can also cause elevated levels.
-
Digital Rectal Exam (DRE) – In this procedure, a doctor inserts a gloved, lubricated finger into the rectum to examine the prostate for any irregularities.
-
Biopsy – If PSA levels or DRE results are abnormal a biopsy may be recommended. A small sample of prostate tissue is removed and examined under a microscope for cancer cells.
-
Imaging Tests – MRI, CT scans, and ultrasound can help determine the extent of the cancer and if it has spread.
Early detection is key. In the USA, the 5-year survival rate for men with localized or regional prostate cancer is almost 100%. But the survival rate plummets if diagnosed at an advanced stage.
According to the World Health Organization, the global 5-year survival rate for prostate cancer is 98% if prostate cancer increases detected early. So, prostate cancer screening is important.
What is Stage 1 Prostate Cancer?
Stage 1 prostate cancer is the earliest stage develop prostate cancer where the cancer is in a small area of the prostate and not detectable by imaging or physical exam. It’s often found incidentally during a prostate biopsy done for another condition. The prognosis for stage 1 prostate cancer is excellent. 100% 5-year survival rate.
What are the Symptoms of Stage 1 Prostate Cancer?
Symptoms of stage 1 prostate cancer are usually none or very mild. Since the prostate cancer diagnosed here is in its early stage and confined to a small area of the prostate gland, it doesn’t cause symptoms. Screening and tests are necessary to detect stage 1 prostate cancer.
What is the First Sign of Prostate Cancer?
One of the first warning signs of prostate cancer is urinary symptoms often difficulty urinating or changes in urinary habits. This can be increased frequency, especially at night, and a weak or interrupted urine flow. These two symptoms of prostate cancer are common but not to be ignored and need a doctor’s attention.
What is the Most Common First Symptom of Prostate Cancer?
The most common first symptom of prostate cancer is usually difficulty urinating. This can be a slow or weak urine flow or the need to urinate more frequently. These changes mean there’s a problem with the prostate that needs to be checked.
What is the First Sign of Prostate Cancer?
The first sign of prostate cancer can be an elevated PSA during a routine blood test or irregularities during a DRE. These early warning signs of prostate cancer will prompt further testing to confirm the risk of prostate cancer.
How is Prostate Cancer Detected Early?
Early detection of prostate cancer involves routine screening with PSA tests and DREs, especially for men over 50 or those with a family history of the disease. If abnormalities are found in screening tests, a biopsy is often conducted to confirm the diagnosis.
Are There Any Silent Symptoms of Prostate Cancer?
Yes, most prostate cancer can have silent symptoms, especially in the early stages. Many men with early-stage prostate cancer experience no symptoms at all, making regular screening essential for early detection.
Early detection of prostate cancer is critical. Men over 50 should have annual PSA tests and DREs. Individuals with a family history of prostate cancer should begin screening earlier, typically between the ages of 40 and 45. If you experience any urinary changes, don’t ignore them—consult your doctor immediately.
Prostate cancer, most prostate cancers, when detected early, have a very high success rate. Advances in imaging and biopsy techniques have made early detection more accurate. It’s important to stay informed and proactive about your health.

Prostate Cancer Disease – Procedures and Treatment Options
Surgical Procedures
When prostate cancer is detected, various treatment options are available depending on the stage and aggressiveness of the cancer, as well as the patient’s overall health. Surgical options for most prostate cancers include:
Radical Prostatectomy
This surgery entails removing the entire prostate gland along with some surrounding tissue. It can be carried out using traditional open surgery or through minimally invasive methods such as laparoscopic or robotic-assisted surgery.
Transurethral Resection of the Prostate (TURP)
This procedure is used to relieve symptoms in advanced cases. It involves removing part of the the prostate gland or tissue to alleviate urinary obstruction.
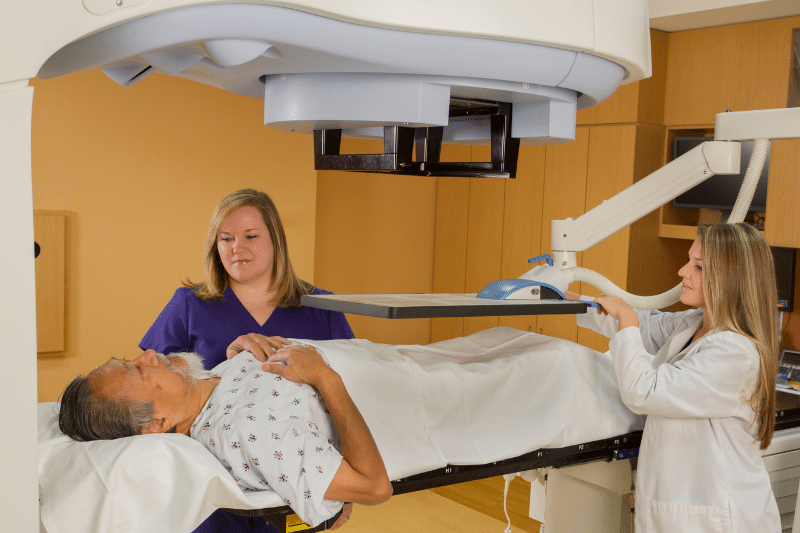
Radiation Therapy
Radiation therapy employs high-energy rays to precisely target and destroy cancer cells. It can be delivered externally or internally (brachytherapy). This treatment is often used for early-stage prostate cancer or as an adjunct to surgery.
Hormone Therapy
Hormone therapy, or androgen deprivation therapy (ADT), internal radiation therapy, seeks to lower the levels of male hormones that may promote prostate cancer growth. This treatment is often utilized for advanced cases of prostate cancer or combined with other therapies.
Chemotherapy
Chemotherapy uses drugs to kill rapidly dividing cancer cells. It is generally employed for advanced prostate cancer that has metastasized beyond the prostate gland and is not responding to hormone therapy.
Immunotherapy
Immunotherapy is targeted therapy that enhances the body’s immune system to recognize and fight cancer cells. This emerging treatment option shows promise for advanced prostate cancer, particularly in cases where other treatments have failed.
Treatment success rates diagnose prostate cancer vary depending on the stage of the cancer at diagnosis. According to the National Cancer Institute, the five-year survival rate for localized prostate cancer is nearly 100%.
For regional prostate cancer, it is about 98%, and for distant-stage prostate cancer screening, the rate drops from very high risk to around 30%. Advances in treatment options continue to improve these outcomes.

Developing Prostate Cancer – Risks and Complications
Potential Risks of Prostate Cancer Treatment
While prostate cancer treatments are generally safe, they can have potential risks and complications. These risk factors may include:
Urinary Incontinence
Some men may experience difficulty controlling urine after prostate surgery or radiation therapy and develop prostate cancer. Consequently, this condition can range from mild leakage to more severe incontinence.
Erectile Dysfunction
Treatments for prostate cancer, particularly surgery and radiation, can affect nerves and blood vessels involved in erections, leading to an increased risk of erectile dysfunction.
Bowel Dysfunction
Radiation therapy can cause changes in bowel habits, including diarrhea, rectal bleeding, or discomfort.
Hormonal Side Effects
Hormone therapy can lead to side effects such as hot flashes, decreased libido, and bone thinning.
Fatigue and Nausea
Chemotherapy and radiation can cause fatigue, nausea, and other systemic effects.
Benefits of Prostate Cancer Treatment
Despite the potential risks, prostate cancer treatments offer significant benefits:
-
Prolonged Survival – Early detection and treatment significantly improve survival rates, with many men living long, healthy lives post-treatment.
-
Symptom Relief – Treatments can alleviate symptoms like urinary obstruction, pain, and discomfort, improving the quality of life.
-
Reduced Risk of Metastasis – Effective treatment reduces the risk of cancer spreading to other parts of the body.
Complication Rates
Evidently, complication rates vary by treatment and patient. For example, 20-30% of men will experience urinary incontinence after radical prostatectomy and 30-50% will have erectile dysfunction. However, with advances in surgical technique and post-op care, those rates have decreased over time.
Prostate Cancer Disease – Available Treatments
Pre-Treatment
Before treatment patients are evaluated to determine the best plan. This may include:
-
Medical History and Physical – Review of patient’s overall health and medical history.
-
PSA and Biopsy – Review of cancer severity and stage.
-
Imaging – MRI, CT, or bone scan to see if cancer has spread.
-
Consultation with Specialists – Discussion of treatment options with urologists, oncologists, and radiologists.
Pre-Surgery
For surgery patients, preparation involves:
-
Pre-Surgical Instructions – Fasting, medication adjustments, and other pre-surgical protocols.
-
Physical Preparation – Good physical health through diet and exercise.
-
Mental Preparation – Understanding the procedure, outcomes, and recovery.
Preparation is key to a good outcome. Additionally, patients should follow their doctor’s instructions, ask questions, and understand the procedure. Being healthy and positive can also make a big difference in recovery.

Prostate Cancer Disease – Post-Treatment and Lifestyle Changes
After Surgery
Recovery time will vary by surgery and patient. Generally, patients can expect to:
-
Hospital Stay – A few days post-surgery for monitoring and initial recovery.
-
Manage Pain – With prescribed meds and follow pain management guidelines.
-
Gradually Resume Activities – Light activities within a few weeks, strenuous activities for at least 6-8 weeks.
Long-Term Care and Monitoring
After treatment follow-up is to monitor for cancer recurrence and long-term effects. This includes:
-
PSA Tests – Blood tests to check PSA levels.
-
Imaging Tests – Scans to check for cancer recurrence or spread.
-
Lifestyle Modifications – A healthy lifestyle, balanced diet, exercise, and stress management techniques.
Diet and Nutrition
A healthy weight and diet are key to recovery of healthy weight, and overall health.
-
Protein Foods – For tissue repair and recovery.
-
Fruits and Vegetables – For vitamins, minerals, and antioxidants.
-
Whole Grains – For energy and digestive health.
-
Hydration – Drink plenty of water to stay hydrated and for body functions.
Physical Activity
Physical activity can help with physical and mental health post-treatment. Gentle exercises like walking, yoga, and swimming can be helpful. But avoid heavy lifting and high-impact activities till fully recovered. Additionally, side effects management is an important part of post-treatment care. This may include:
-
Pelvic Floor Exercises – To improve urinary control and reduce incontinence.
-
Medications and Therapies – For erectile dysfunction or hormonal side effects.
-
Support Groups and Counseling – For emotional support and coping strategies.

Prostate Cancer Disease – Research and Advances in Treatment
Latest Research
Research is ongoing to improve our understanding and treatment of advanced prostate cancer further. Some recent developments in prostate cancers are:
- Immunotherapy Advances – Boosting the immune system to fight cancer.
- Targeted Therapies – Developing drugs that target cancer cells without harming healthy tissue.
- Genetic Testing – Identifying genetic mutations that increase the risk of prostate cancer and tailoring treatment accordingly.
Clinical Trials
Joining a clinical trial can give you access to the latest treatment and contribute to medical knowledge. Subsequently, individuals should discuss with their doctor to see if they are eligible and what are the benefits. However, the future of prostate cancer treatment looks good, with research focused on:
-
Personalized Medicine – Tailoring treatment according to individual genetic and molecular profiles.
-
Better Diagnostic Tools – Developing more accurate and noninvasive methods for early detection.
-
New Treatment Modalities – Combining different therapies for better outcomes and fewer side effects.

Prostate Cancers FAQs
How to Stop Prostate Cancer?
You can’t prevent prostate cancer or always stop prostate cancer but you can reduce the below risk factors:
-
Healthy Diet – Fruits, veggies, and healthy fats.
-
Regular Exercise – Being active.
-
No Smoking – Reducing carcinogens.
-
Regular Screening – Especially if you’re at higher risk due to family history.
Genetics and Prostate Cancer
Genetics plays a big role in prostate cancer risk. Similarly, men with a family history of prostate cancer or genetic mutations like BRCA1 and BRCA2 have a higher risk of developing prostate cancer. In fact, Genetic counseling and testing can help identify these risks and guide prevention.
Mental Health During Treatment
Mental health is key during cancer treatment. Stress, anxiety, and depression can affect recovery and overall well-being. Additionally, seek support from mental health professionals, join support groups, and practice stress relief techniques to manage these challenges.
Diet and Prostate Cancer Management
A balanced diet is overall health and recovery during prostate cancer treatment. However, foods rich in antioxidants, vitamins, and minerals can boost the immune system and treatment outcomes. Avoiding processed foods, red meat, and high-fat foods can also benefit prostate health.
Imaging and Diagnostic Advances
Recent advances in imaging and diagnostic tools have improved prostate cancer detection and staging. In particular, multiparametric MRI, PET scans, and advanced biopsy can provide more detailed information about the often developing symptoms of prostate cancer and help with treatment planning.
Holistic Prostate Cancer Care
Certainly, adding holistic approaches like acupuncture, meditation, and nutritional supplements can complement conventional treatments and improve quality of life. But always discuss these with your healthcare provider to ensure they are safe and effective. Moreover, prostate cancer treatment has come a long way. We have better and less invasive options now that yield better results and fewer side effects. Nonetheless, individuals developing prostate cancer should be informed and involved in their care.

Key Differences Between Colonoscopy and Prostate Exam
Does Colonoscopy Check for Protract Cancer?
Surgeons perform colonoscopy to detect colon cancer and other conditions affecting the colon. However, it is not used to check for prostate cancer. A colonoscopy examines the inner lining of the colon and rectum. Primarily used for detecting colorectal cancer, polyps, and other colon-related conditions. The procedure involves the insertion of a colonoscope into the rectum, usually under sedation. Generally recommended every 10 years starting at age 50 for those at average risk of colorectal cancer, or more frequently if there are risk factors or previous findings.
While prostate exam assesses the health of the prostate gland. Mainly used for detecting symptoms of prostate cancer and other prostate-related conditions. Includes a Digital Rectal Exam (DRE) and/or a Prostate-Specific Antigen (PSA) blood test, both of which are quick and typically do not require sedation. The frequency of DRE and PSA tests varies based on individual risk factors. But annual exams may be recommended for men over 50 or earlier for those at higher risk.











