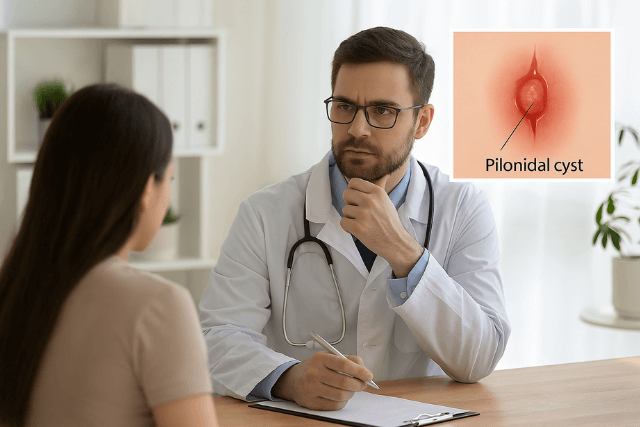
Pilonidal disease is a painful and recurring skin condition that typically occurs near the tailbone. Often affecting young adults, especially men, it involves the formation of a cyst or abscess in the cleft between the buttocks. Hair, debris, and bacteria can collect in this area, causing inflammation and infection. Without proper pilonidal disease treatment, the condition can persist, returning repeatedly and disrupting daily life.
Fortunately, there are several treatment options available today that offer fast relief and long-term healing. From conservative care to advanced laser therapies like Sinus Laser-Assisted Closure (SiLaC®), patients now have access to solutions that reduce downtime and improve quality of life.
Understanding the Symptoms of Pilonidal Disease
Before diving into the best pilonidal disease treatment options, it’s important to first understand the common symptoms. After all, recognizing the signs early often leads to a quicker diagnosis and faster relief. In many cases, knowing what to watch for can help you take action before the condition worsens.
Common Symptoms of Pilonidal Disease
- Pain or discomfort near the tailbone
- Swelling or redness in the lower back area
- Pus or blood draining from a small hole in the skin
- A foul smell from the discharge
- Tenderness while sitting or moving
These symptoms can develop gradually. However, they often become more noticeable after long periods of sitting or physical activity. In addition, poor hygiene or excessive sweating may cause the condition to flare up more quickly.
If you experience any of these symptoms, early evaluation is absolutely critical. Therefore, do not delay in seeking medical advice. With the right pilonidal disease treatment, you can not only relieve discomfort but also prevent further complications and lower the risk of recurrence.
Causes and Risk Factors
Pilonidal disease doesn’t happen randomly. Several known risk factors make some people more susceptible than others.
Risk Factors Include:
- Sitting for long periods
- Excess body hair
- Friction from tight clothing
- Poor hygiene
- Obesity
- A family history of the condition
Because of these triggers, a comprehensive pilonidal disease treatment plan often includes lifestyle changes to prevent recurrence alongside medical or surgical interventions.
Treatment Goals for Pilonidal Disease
Effective treatment must do more than just manage symptoms. It should aim to:
- Eliminate the existing infection
- Promote quick wound healing
- Minimize recurrence
- Reduce scarring and recovery time
With these goals in mind, let’s explore the best treatment options available today.
Non-Surgical Pilonidal Disease Treatment Options
For mild cases or early-stage pilonidal disease, non-surgical methods may offer relief. While these methods may not work for everyone, they can be highly effective when symptoms are minimal.
1. Conservative Care
Conservative care focuses on hygiene, hair removal, and lifestyle changes.
Key strategies:
- Shaving or laser hair removal around the affected area
- Keeping the area clean and dry
- Using warm compresses to ease inflammation
- Avoiding long periods of sitting
While these methods can’t cure deep or recurring infections, they can be part of a maintenance plan after other treatments.
2. Antibiotics
If there’s an active infection but no abscess, doctors may prescribe antibiotics. However, it’s important to note that antibiotics alone don’t typically cure the disease because they can’t remove the sinus tract. Still, they play a helpful role in controlling flare-ups.
Minimally Invasive Treatment for Pilonidal Disease
Minimally invasive options are changing the game in pilonidal disease treatment. These techniques often involve less pain, faster healing, and minimal scarring compared to traditional surgery.
1. Sinus Laser-Assisted Closure (SiLaC®)
SiLaC® is a cutting-edge technique that uses laser energy to destroy the pilonidal sinus tract from the inside out. This is one of the most advanced and promising forms of treatment available today.
Benefits of SiLaC® include:
- Quick recovery (usually within days)
- Minimal pain after the procedure
- Reduced risk of recurrence
- No large open wounds
- Can often be done under local anesthesia
SiLaC® works by inserting a laser fiber into the tract and sealing it closed as the laser is withdrawn. As a result, the sinus tract collapses, and the body naturally heals the area. It’s ideal for people seeking a long-term solution with minimal downtime.
2. Pit-Picking Procedure
Another minimally invasive method is pit picking. In this procedure, a surgeon removes the small openings (pits) and cleans the tract using small incisions.
Advantages:
- Short recovery time
- Performed under local anesthesia
- Can be done in an outpatient setting
However, pit picking may not be suitable for patients with large or complex sinus tracts.
Surgical Pilonidal Disease Treatment
For chronic or severe cases, surgery may be necessary. Surgical options vary in complexity, but they aim to remove the entire sinus tract to prevent recurrence.
1. Excision with Healing by Secondary Intention
This involves removing the affected tissue and leaving the wound open to heal naturally.
Pros:
- Low risk of recurrence
- Allows the wound to drain completely
Cons:
- Long healing time (several weeks to months)
- Requires daily wound care
- Can be painful during recovery
2. Excision with Primary Closure
Here, the surgeon removes the tract and then stitches the skin closed.
Pros:
- Faster healing time
- Less wound care required
Cons:
- Slightly higher risk of recurrence
- Risk of wound infection or opening
3. Flap Surgery (e.g., Bascom Cleft Lift)
For patients with multiple recurrences or wide sinus tracts, flap surgery may be the best option. This involves reshaping the affected area and repositioning skin to reduce tension and improve healing.
Benefits:
- High success rate
- Better cosmetic results
- Lower recurrence rate in experienced hands
Comparing the Best Options
Let’s compare all available options based on key factors:
| Treatment Type | Recovery Time | Pain Level | Recurrence Risk | Scarring | Setting |
|---|---|---|---|---|---|
| SiLaC® (Laser) | 3–5 days | Low | Low | Minimal | Outpatient |
| Pit-Picking | 3–7 days | Low | Medium | Minimal | Outpatient |
| Antibiotics | Immediate | Low | High | None | Outpatient |
| Open Surgery | 4–8 weeks | High | Low | High | Inpatient/Daycare |
| Flap Surgery | 2–4 weeks | Medium | Very Low | Moderate | Surgical Center |
Clearly, SiLaC® stands out as a strong option for those wanting both speed and long-term success. However, the best choice depends on the severity of your condition and your doctor’s recommendation.
Recovery Tips for Faster Healing
No matter which pilonidal disease treatment you choose, proper aftercare is essential. Here are some simple tips to help you heal faster:
- Keep the area clean and dry. Gently wash with mild soap and water daily.
- Avoid sitting for long periods. Use a cushion if needed.
- Follow wound care instructions. Change dressings as advised.
- Remove hair regularly. Use shaving or laser hair removal to prevent hair buildup.
- Stay active. Light walking can boost circulation and promote healing.
These steps may seem small, but they can make a big difference in your recovery.
How to Prevent Recurrence
After successful pilonidal disease treatment, your next focus should be on preventing the condition from coming back. Thankfully, this doesn’t have to be difficult. In fact, with just a few small lifestyle changes, you can lower your risk of recurrence significantly.
Make hygiene a top priority. In addition, avoid wearing tight-fitting clothes that create friction around the tailbone area. Furthermore, keeping the area clean and free of hair plays a vital role in stopping the problem before it starts.
Here are some essential steps to follow:
- Maintain good hygiene to keep bacteria and debris away
- Avoid tight-fitting clothes that cause irritation
- Keep the area hair-free, using shaving or laser removal
- Stay at a healthy weight to reduce pressure on the area
- Don’t ignore early symptoms, even if they seem mild
If you’ve already had pilonidal disease treatment and the symptoms come back, don’t delay. Instead, talk to your doctor right away. Prompt action, especially early intervention, can prevent more serious complications from developing later.
When to See a Specialist
Unfortunately, some people live with recurring symptoms for months or even years without seeking proper treatment. As a result, their condition often becomes more severe. For this reason, it is important to know when to seek professional help. If any of the following signs apply to you, it is time to consult a specialist:
Frequent flare-ups
- Pain that interferes with your daily activities
- Persistent drainage or an unpleasant smell
- No improvement with home care
In situations like these, delaying treatment can lead to further discomfort and complications. Therefore, taking action sooner rather than later can greatly improve your outcome. By visiting a colorectal surgeon or a skin specialist, you will receive a complete evaluation and a targeted pilonidal disease treatment plan designed specifically for your condition.
Early specialist care not only speeds up healing but also lowers the chances of recurrence.
Conclusion: Pilonidal Disease Treatment
Ultimately, finding the right pilonidal disease treatment does not have to be overwhelming. In fact, with a wide range of options available, including conservative care and advanced laser treatments like SiLaC®, there is a solution for every patient. To begin with, early diagnosis plays a critical role in effective healing. In addition, making informed decisions and staying consistent with aftercare can significantly improve your recovery.
On one hand, minimally invasive methods are becoming more popular because they offer quick results, less pain, and minimal scarring. On the other hand, traditional surgeries are still reliable when dealing with more serious or recurring cases. Therefore, it is essential to understand each option and consult a qualified medical provider before making a final choice.
At the end of the day, no matter which treatment path you follow, the goal should always be long-term relief and better quality of life. After all, your health and comfort are what matter most. Although pilonidal disease can be persistent, with the right treatment and ongoing care, you can confidently return to a pain-free and active lifestyle.