Gastrectomy – Definitions and Medical Terms
What does gastrectomy mean?
In medical terms, gastrectomy means removing all or part of the stomach. The healthcare providers perform laparoscopic gastrectomy to treat stomach cancer. Often including the removal of nearby lymph nodes. But can also perform to treat peptic ulcers, benign tumors, and severe obesity.
What is the suffix in gastrectomy?
The suffix in gastrectomy is “-ectomy” which means the first surgical procedure or removal of a part of the body. The prefix “gastro-” means the entire stomach itself. So gastrectomy means the removal of the entire stomach itself.
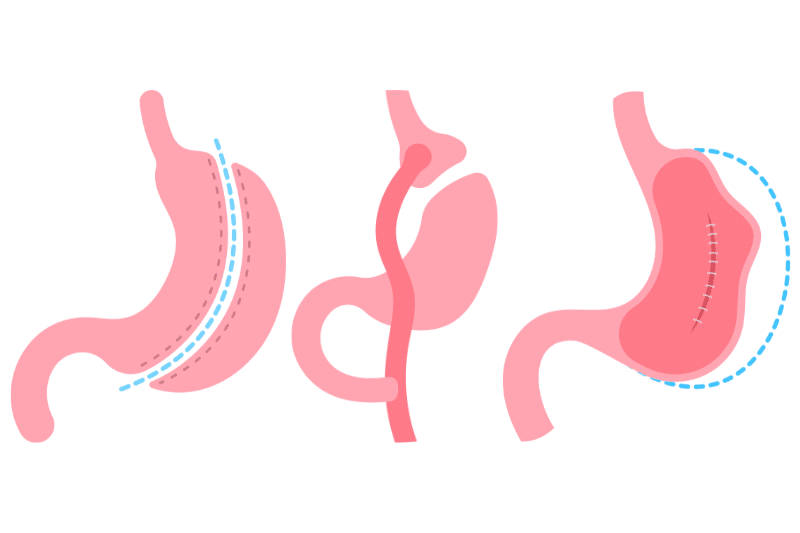
What is total gastrectomy?
Total gastrectomy means removing the whole stomach. This is often necessary for patients with advanced stomach cancer. The healthcare provider connects the esophagus to the small intestine so the individual can eat. As a matter of fact, this is a big deal for the digestive system and requires major lifestyle changes.
What is the medical term for removing part of the stomach?
The medical term for removing part of the stomach is partial gastrectomy (subtotal gastrectomy). This is removing only the diseased or damaged part of the stomach leaving the rest intact. It is less invasive than total gastrectomy. Particularly used for localized conditions.
What is stomach excision called?
Doctors refer to stomach excision as gastrectomy. Depending on how much doctors surgery to remove. Either it’s partial gastrectomy (part of the stomach) or total gastrectomy (whole stomach).
What is partial stomach removal called?
Doctors refer to partial stomach removal as a partial gastrectomy. This is removing a part of the abdomen or stomach, usually where the tumor or diseased tissue is. Then, the rest of the abdomen or stomach connected to the intestine to continue digestive functions.
Gastrectomy – Medical Reasons and Indications
Why do people get gastrectomies?
People get gastrectomies for stomach cancer. According to the American Cancer Society, 27,600 people diagnosed with stomach cancer in the US in 2023. This is also for peptic ulcers that don’t respond to other treatments. Furthermore caused by benign stomach tumors and severe obesity. Particularly, when other weight loss methods fail.
Why would you need a gastrectomy?
You might need a gastrectomy if you have:
Severe Peptic Ulcers
Remove ulcerated tissue that won’t heal with medication.
Stomach Cancer
When cancer is widespread and other treatments don’t work.
Obesity
As a last resort for severe obesity, it helps with significant weight loss.
Severe Trauma
In cases of severe abdominal injury where the stomach is beyond repair.
Benign Tumors
To remove non-cancerous growths that could cause problems if left untreated.
Gastrointestinal Stromal Tumors (GISTs)
Large or problematic GISTs may require partial or total removal of the stomach.
Hereditary Diffuse Gastric Cancer
People with this genetic condition are at high risk of stomach cancer. May have a prophylactic total gastrectomy to prevent cancer. Individuals with harmful CDH1 mutations may consider preventive gastrectomy to reduce the risk of developing stomach cancer.
Gastrectomy is a life-saving procedure for many. But comes with big lifestyle changes and potential complications. Nevertheless, knowing these is important if you’re considering or preparing for this major surgery.
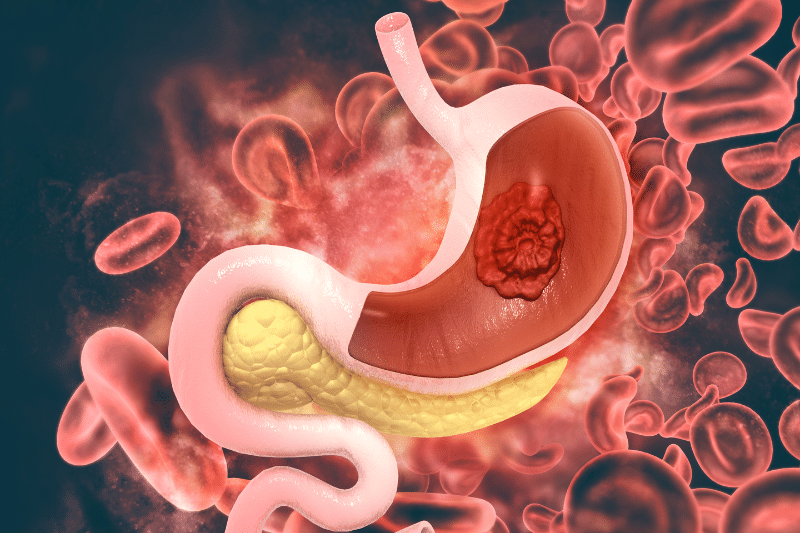
Gastrectomy – Stomach Cancer Risks in the USA
Stomach cancer, also known as gastric cancer. Starts in the stomach lining and can spread to other parts of the body.
The American Cancer Society estimates in 2023. There will be 27,600 new cases of stomach cancer in the US and 11,010 will die from the disease.
Stomach cancer is most common in older adults, the average age of diagnosis is 68. The 5-year survival rate varies by stage, from 68% for localized to 5% for the advanced stage. Early detection is hard because cancer symptoms are subtle and often late-stage diagnosis.
Risk Factors Developing Stomach Cancer
These are the risk factors for stomach cancer:
Smoking
Smoking doubles the risk of developing stomach cancer. Tobacco smoke contains carcinogens that can damage stomach cells.
Helicobacter Pylori Infection
This bacterial infection is a major cause of stomach ulcers and can lead to chronic inflammation and increased cancer risk.
Family History
Having a family history of stomach cancer increases your risk. Genetic predisposition and shared lifestyle factors contribute to this increased risk.
Diet
Eating a diet high in smoked, salted, and pickled foods increases the risk of stomach cancer. These foods contain nitrates and nitrites which can damage the stomach lining.

How to reduce stomach cancer risks?
Dietary changes
A healthy diet can reduce the risk of stomach cancer:
More Fruits and Veggies
Eating a diet rich in fresh fruits and veggies gives you the vitamins, minerals, and antioxidants to fight cancer.
Less Processed Foods
Reducing processed and smoked foods reduces the amount of carcinogens you ingest.
Healthy Cooking Methods
Grilling, steaming, and boiling instead of smoking and frying help retain nutrients and reduce harmful substances.
Lifestyle changes
Add these lifestyle changes to further reduce the high risk of stomach cancer:
Limit Alcohol – Moderate alcohol consumption reduces the risk of stomach and other cancers.
Quit Smoking – Stopping tobacco use reduces the risk of many cancers including stomach and breast cancer.
Exercise Regularly – To maintain a healthy weight and reduce breast cancer risk.
Medical Check-ups
Regular monitoring and early detection are key to effective treatment and better outcomes.
H. pylori Screening – Early detection and treatment of H. pylori can prevent ulcers and reduce cancer risk.
Genetic Testing – Those with a family history of stomach cancer may benefit from genetic testing and counseling. To further assess their risk and take preventive measures.
Knowing gastrectomy, its implications, and preventive measures for stomach cancer is important for anyone going through this major surgery. By making healthy dietary and lifestyle changes you can reduce your risk of developing stomach cancer symptoms.
Lastly, informed treatment decisions and proactive measures can make a big difference in managing health risks and living better.
Gastrectomy or Partial Gastrectomy – Organs and Functions
What organ is removed during a gastrectomy?
During a gastrectomy, the entire stomach itself is removed either partially or totally. This is a major operation usually done for stomach cancer, severe peptic ulcers, or other major stomach problems. In total gastrectomy, the doctor removes the whole stomach. Along with nearby lymph nodes to test for the spread of cancer and ensure its thorough removal. Whereas in partial gastrectomy, it’s the only affected part of the stomach.
What functions are lost in a patient who has total gastrectomy?
When the surgeon removes the whole stomach (lymph nodes). Then the body loses:
Digestion and Food Storage
The stomach’s main job is to store and digest food and start the digestion process. Moreover, breaking down food with stomach acid and enzymes. Without a stomach, the individual loses this storage capacity so they will have to eat smaller more frequent meals.
Nutrient Absorption
The stomach is also responsible for absorbing certain nutrients, especially vitamin B12. Without a stomach patients often need vitamin B12 injections or supplements because their body can no longer absorb this vitamin.
What happens to the stomach after gastrectomy?
After a gastrectomy, open surgery where the surgeon connects the esophagus to the small intestine. The surgeon makes open surgery for this connection as an esophagojejunostomy. Food will pass from the esophagus to the small intestine.
While this allows digestion to continue it changes the process. Thus, they will have to adapt to the liquid diet regime. Even supposing they may experience digestive problems.
Stomach Gastrectomy – Major Surgery Procedures and Types
Is gastrectomy a big surgery?
Yes, gastrectomy is a big surgery. It’s a big deal with the digestive system and requires a lot of consideration and post-op care. In fact, the surgery can take hours in the operating room. They will be in the hospital for several weeks to about a quarter week or more. Eventually depending on how they will recover faster.
What’s partial stomach removal called?
Partial stomach removal surgery is called partial gastrectomy. This is less invasive than total gastrectomy and only removes the diseased or damaged part of the stomach.
The remaining part of the stomach is then reconnected to the digestive tract. Afterward, they can still retain some of the entire stomach’s natural function.
Gastrectomy – Reproductive Health
Can you have a baby after gastrectomy?
Yes, you can have a baby after gastrectomy but there are important considerations to keep in mind:
Nutritional Challenges
Pregnancy increases the body’s nutritional demands. Since gastrectomy patients may have difficulty absorbing certain nutrients. Therefore, you need to work closely with your healthcare provider to ensure proper nutrition.
Monitoring and Medical Support
Regular monitoring and medical support are crucial for a healthy pregnancy post-gastrectomy. This full care team includes frequent doctor check-ups, dietary adjustments, and potentially additional supplements for the mother and the baby.

Gastrectomy – Life After Surgery and Adjustment
What’s life like after a gastrectomy?
Life after a gastrectomy is a big adjustment. To digest food, the stomach should adept for nutrient absorption. Without it, they have to adjust to new food habits and diets. Eating smaller more frequent meals is necessary.
Patients may feel sick and experience changes in their digestive system. Subsequently, may feel sick and get dumping syndrome where food moves too fast from the stomach to the small intestine. Consequently, it can cause nausea, diarrhea abdominal pain, and dizziness.
Can you live a normal life after a gastrectomy?
Yes, you can live a normal life after a gastrectomy but it’s an adjustment. You have to focus on nutrition and follow a diet suitable for your new digestive system.
Regular checkups with healthcare providers will ensure nutritional deficiencies are addressed. Many people can still have a good quality of life post-surgery by managing their diet and lifestyle.
What happens when the stomach is removed?
When the surgeon removes the stomach. Either partially or totally, the digestive process changes. In a total gastrectomy, the esophagus is connected directly to the small intestine. Thus, the stomach’s role in breaking down food and regulating its release into the intestine is lost.
The patient has to eat smaller meals more frequently and take supplements. To further compensate for the nutrients the stomach would normally absorb from certain medicines like vitamin B12.
What happens when you have a total gastrectomy?
Firstly, the surgeon removed the whole stomach. Then the esophagus connected to the small bowel. Although, this is often necessary for advanced stomach cancer.
Post-surgery patients need to follow a strict diet of soft food. Besides this, they need regular checkups to monitor their nutritional status and overall health.
What happens when you have a gastrectomy?
When you have a gastrectomy the surgeon removes part or all of the stomach. Especially depending on the extent of the disease. Lastly, recovery involves getting used to a new clear liquid diet and monitoring for complications.
Such as infections or nutrient deficiencies. As a result, patients lose weight initially. Later they need to work with a dietitian to ensure they get enough nutrition.
What happens when the stomach is removed?
When the stomach is removed the digestive process is changed. The esophagus is connected to the small bowel, the food pipe bypassing the stomach. This means the individuals have to get used to new eating habits and dietary restrictions.
The body can no longer store and release food slowly. Therefore, individuals have to eat smaller meals throughout the day. So as not to overwhelm the digestive system.
What happens when they remove some of your stomach?
When they remove part of your stomach, the remaining bottom part of your stomach is attached to the digestive tract. You will still have some stomach function. But must adjust your food intake habits. To switch to a clear liquid diet.
However, you may experience acid reflux or dumping syndrome. Further need to follow your doctor and dietary recommendations to manage these.
Gastrectomy – Life Expectancy and Outcomes
How long do you live with a gastrectomy?
Life expectancy with a gastrectomy varies depending on several factors. For instance, the reason for the surgery, your overall health, and how well you adjust to the new diet.
For those who have gastrectomy for cancer, early detection and treatment make a big difference. Regular follow-ups and a healthy lifestyle are key to better long-term outcomes.
Gastrectomy – Weight Loss Procedures
What are the safest weight loss procedures if you have had a gastrectomy?
Having a gastrectomy affects your digestive system and overall health. When looking at weight loss procedures post gastrectomy. Although, you need to choose options that are safe for your altered digestive anatomy. Here are the safest weight loss procedures for most people, who have had a gastrectomy:
1. Sleeve Gastrectomy
Remove a large part of the stomach, leaving a banana-shaped sleeve. Restrictive procedure that limits food intake. Conversely, not digesting food is suitable for those who have post-gastrectomy. Because the doctor already removed most of the other stomach tissue.
2. Gastric Bypass (Roux-en-Y)
The pouch is created from the stomach and connected to a feeding tube in the small intestine. Suitable for partial gastrectomy patients as it reduces stomach size and absorption of digested food. However, not suitable for total gastrectomy patients.
3. Adjustable Gastric Band
Band around the upper part of the stomach to create a small pouch to limit food intake. Surely, not suitable for post-gastrectomy patients as stomach anatomy is already altered.
4. Endoscopic Sleeve Gastroplasty
Minimally invasive procedure where the doctor places the sutures in the stomach to reduce its size. Certainly, suitable for partial gastrectomy patients. However, a specialist doctor may evaluate it thoroughly. Especially based on the medical history of the patient.
5. Diet and Exercise Programs
Medically supervised programs on diet and exercise tailored to individual needs. Suitable for all post-gastrectomy patients. Manage weight without surgical risks.
Gastrectomy – Recommended Procedures
Which weight loss procedure is suitable for individuals who have undergone gastrectomy surgery?
Stomach issues or gastrectomy patient
s need special care when it comes to treatment for weight loss procedures. Suitable treatment for each patient, surgery depends mostly on health condition and type of gastrectomy.
Medical Procedures
Pharmacotherapy
-
Medications to help with weight loss by suppressing appetite or reducing fat absorption. For example, Orlistat, Phentermine-Topiramate. Suitable for partial gastrectomy patients. Monitor for side effects.
Surgical Procedures
Gastric Bypass (Roux-en-Y)
-
Small stomach pouch and rerouting of small intestine. Suitable for partial gastrectomy patients. Risks include nutritional deficiencies and dumping syndrome.
Endoscopic Sleeve Gastroplasty
-
Healthcare provider places sutures endoscopically to reduce stomach size. Suitable for partial gastrectomy patients. Associated risks are – less invasive but require special evaluation.
Non-Surgical Procedures
Medically Supervised Diet and Exercise
-
Customized diet plans and exercise regimens. Suitable for all gastrectomy patients. Benefits include – non-invasive, tailored to the individual.
Behavioral Therapy
-
Counseling and behavioral modifications to support weight loss. Suitable and beneficial for all patients. Furthermore, it addresses psychological aspects of eating and weight.
What are the advantages and disadvantages of these weight loss procedures?
Pharmacotherapy
-
Benefits – Non-invasive, can work with lifestyle changes.
-
Considerations – Side effects, not for long-term use, require medical care team supervision.
Gastric Bypass (Roux-en-Y)
-
Benefits – Weight loss, improves obesity-related conditions.
-
Considerations – Surgery, complications (nutritional deficiencies, dumping syndrome).
Endoscopic Sleeve Gastroplasty
-
Benefits – Minimally invasive, shorter recovery time, fewer complications.
-
Considerations – Limited long-term data, not for everyone, suture-related issues.
Medically Supervised Diet and Exercise
-
Benefits – Safe, holistic approach, overall health improvement.
-
Considerations – Long-term commitment, slower weight loss than surgery.
Behavioral Therapy
-
Benefits – Addresses psychological issues, long long-term weight management.
-
Considerations – Regular sessions, results vary with individual commitment.
What are the considerations, risks, and ideal and non-ideal candidates?
Considerations
-
Medical History – Full medical history and current health status.
-
Nutritional Status – Nutritional deficiencies and supplementation requirements.
-
Lifestyle Factors – Willingness and ability to follow dietary and lifestyle changes.
-
The Extent of Gastrectomy – The type of gastrectomy (partial or total) determines suitability.
Risks
-
Surgical Risks – Infection, bleeding, blood clots, anesthesia-related complications.
-
Digestive Issues – Dumping syndrome, bowel changes, and absorption problems.
-
Nutritional Deficiencies – Vitamins and minerals deficiencies that will require lifelong supplementation.
Ideal Candidates
-
Committed – Willing to follow lifestyle changes and medical advice.
-
Good Health – No significant comorbidities that increase surgical risks.
-
Partial Gastrectomy Patients – Suitable for some surgical and nonsurgical weight loss options.
Non-Ideal Candidates
-
Non-Compliant – Unlikely to follow dietary and lifestyle changes.
-
Total Gastrectomy Patients – Limited surgical weight loss options.
-
Poor Surgical Candidates – Significant medical issues that increase surgical risks.
Gastrectomy – Eating and Nutrition Post-Surgery
Can you eat if you have had your stomach removed?
Yes, you can eat if you have had part of your stomach removed. Though it requires big changes in how you eat and what you eat. Since the stomach is a major part of digestion. Furthermore, having it remote and stopping to stop eating as often means. Finally, you have to adapt to a new way of eating.
How do you eat after a total gastrectomy?
After a total gastrectomy, you need to follow specific dietary guidelines to get proper nutrition and avoid complications. The small intestine takes over some of the stomach’s function but it needs smaller more frequent meals to manage digestion.
Meal Size and Frequency
-
Small Meals – Eat smaller portions more frequently, 6-8 times a day.
-
Chew Thoroughly – Chewing food thoroughly helps with digestion as the stomach’s mechanical breakdown is no longer available.
Nutritional Supplements
-
Iron and Calcium – May need supplementation to prevent deficiency.
-
Vitamin B12 – Since the stomach is responsible for absorbing vitamin B12. Individuals need lifelong B12 injections or supplements.
Food Choices
-
Easy to Digest – Doctors recommend soft foods, purees, and liquids first.
-
Balanced Diet – Then a diet rich in proteins, vitamins including (vitamin E), and minerals is key.

Gastrectomy – Dietary Guidelines
How do people eat with a gastrectomy?
People who have had a gastrectomy adjust to eating with their new digestive system. Hence, means big changes to their lifestyle to get enough nutrition and avoid complications.
Dietary Changes
-
High-Protein Foods – Lean meats, fish, and legumes.
-
No Sugars and Fats – No sugars and fats to avoid dumping syndrome.
-
Hydration – Drink plenty of fluids but not with meals to not overwhelm the system.
Monitoring and Adjustment
-
Check-Ups – Regular medical check-ups to monitor nutrition and adjust the diet.
-
Personalized Diet Plans –Work with dietitians to create personalized meal plans.
Can you eat with a total gastrectomy?
Yes, you can eat with a total gastrectomy. But you must follow the diet strictly and monitor regularly to get enough nutrition. Moreover, the small intestine can adapt to some of the stomach’s functions. But it takes time and management.
What do I eat after total gastrectomy?
Eating after total gastrectomy is a gradual process of progression. From a liquid diet to more solid foods except for od pipe and foods to solids.
Stage 1
-
Full Liquids – Smoothies and soups.
-
Clear Liquids – Water, broth, clear juices post-op.
Transition
-
Pureed Foods – Blended foods.
-
Soft Foods – Mashed potatoes and scrambled eggs.
Maintenance
-
Regular Foods – Reintroduce regular foods and small frequent meals.
-
Ongoing Monitoring – Adjust as needed based on tolerance and nutritional needs.
Indeed, gastrectomy is a big surgery with big implications for diet and nutrition. Nonetheless, at IBI Healthcare our medical and care team ensures that patients are well informed. Knowing the safest weight loss procedures and adapting to new eating habits post-surgery is key.
Not only to be healthy but also complication less pain-free. Call us or schedule a teleconsultation. Above all, our experienced surgeons will help you with the procedure details. As well as create a customized plan for you. To follow the pre and post-operative guidelines.











